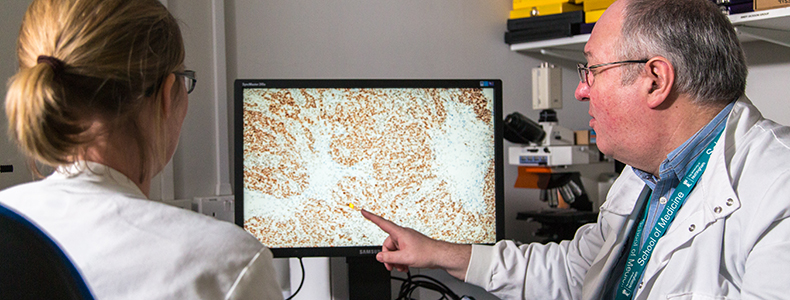
At the lab bench
Thanks to your support for Nottingham Life Cycle 6, our breast cancer research is making good progress. We asked some of our leading breast cancer researchers to share how your gifts are helping them make the next breast cancer breakthrough, faster.
Stopping the spread
Professor Stewart Martin, Nottingham City Hospital
When I look back at the breast cancer research open day we held in 2016, I feel quite humbled. As a scientist, my team and I don’t often have the chance to interact with breast cancer patients and donors. When we get the opportunity it is extremely motivating for us. I was fortunate to receive funding for my research area thanks to the support for Nottingham Life Cycle 6.
Our aim is to help stop breast cancer from spreading around the body and to increase the effectiveness of cancer treatments. We are focusing on a family of proteins called Calpains and have some exciting data coming through. It takes a long time to get laboratory research up and running. Yet, we have now proved that Calpains and related proteins play a key role in making breast cancer cells more aggressive. We first discovered this using samples taken from patients in Nottingham – we verified these initial findings using samples from around the UK.
"Without Life Cycle 6 funding there is no way we would be at the stage we are today."
The main protein we are interested in is Calpastatin. These proteins are not just interesting to breast cancer researchers, but also to those investigating other cancers, cardiovascular diseases and neurodegenerative disorders like Alzheimer’s. We are the first group in the world to clone all the different types of Calpastatin and show where they are within the cancer cells.
We used our Nottingham Life Cycle 6 funding to appoint a new research technician, Holly Nicholls, to help drive this research forward. PhD studentships and peer-reviewed research grants have supplemented this funding and now there’s a dedicated team looking at two approaches. We can remove the protein, using a process akin to gene-editing, then look to see what this does to the cell.
We have also made cells that over-produce the protein and discovered that different Calpastatins regulate cell behaviour in different ways. Now, we are focusing on identifying which ones are most important for therapy resistance and metastasis.
This research is gathering pace and profile. We presented at an international Calpain conference in the USA and since then we’ve developed many exciting collaborations. With partnerships now in place, we’re increasing the chances of finding the breakthroughs faster.
Later this year, we will be applying for grants to take the next steps towards real-world clinical application. Without Life Cycle 6 funding there is no way we would be at the stage we are today. You gave us the chance to focus attention on the most important areas, so on behalf of all the team, thank you.
Tackling triple negative breast cancer
Professor Srinivasan Madhusudan, Nottingham City Hospital
I am delighted to report that we are just about to submit our research paper focused on the role of the XRCC1 protein in triple negative breast cancers (TNBC). Triple negative breast cancers currently have no targeted treatment available – that’s something we are working hard to change.
We discovered that one in five women with TNBC will have a deficiency in the XRCC1 protein. Since the publication of our research, the first of its kind in this area, other researchers have now verified our findings.
We used our Nottingham Life Cycle 6 grant to explore how we can target XRCC1 deficient breast cancers with new personalised treatment. We looked at how different drugs block different DNA repair proteins. They stop the cancer cell from repairing itself after treatment.
We initially focused on Olaparib, a drug that has recently been approved for use in a rare type of breast cancer. We tested Olaparib in XRCC1 deficient breast cancers and proved that the cancer cells do respond.
It is a strong result and means that we are now pushing for a phase 2 clinical trial. This will be my team’s focus for the year. My hope is that we can bring Olaparib to more patients and help more women with this important drug.
This is only one part of our research. We are exploring two other drugs currently under early phase human trials. They also work by blocking the DNA repair mechanisms of the cancer cells. We have completed testing in our initial models where we use cell lines grown from tissue cultures in the laboratory. One drug is looking promising, showing some striking results in XRCC1 deficient breast cancers. Our next step will be to test using more advanced models which better mimic what results we could expect from human patients.
My hope is that we can bring Olaparib to more patients and help more women with this important drug.
A phase 2 clinical trial is an important step in moving our research from the laboratory to the real world through clinical application. It can improve the lives of women around the world and that’s exactly what I want to see happen.
Detecting breast cancer early
Professor John Robertson, Royal Derby Hospital
Work on the world’s first blood test to detect breast cancer is progressing well. This is a really exciting time for us. With each step, we get closer to bringing this innovative new development into the real-world. Our blood test works by detecting the microscopic antibodies our bodies produce when cells start to mutate and become cancerous. It means that we can detect and treat cancers before they grow and spread, helping save the lives of thousands of women around the world.
We have been undertaking a robust testing programme. In a pilot study, our test correctly identified breast cancer in 57% of samples, known as the test’s sensitivity. The test also showed 85% for specificity, which means that false positives occurred in 15% of samples.
In a sub-group including a new cancer antigen, the results were even better – 67% sensitivity and 93% specificity. This means that we are able to detect two-thirds of breast cancers through the blood test – an amazing result.
We are now focusing on repeating this pilot study to double-check our results, before we launch a large scale validation study. But research is expensive – for our repeat study, 60 tumour antigens will cost £30,000. That is for one relatively small repeat experiment, but these costs are necessary at this pivotal stage in our research development.
We have also run a small pilot study on samples taken from patients treated with the anti-cancer drug, Tamoxifen. We wanted to see if we can predict those who will respond. The data for this study is now with our statisticians and we are waiting for their initial analyses.
I am exceptionally grateful to everyone who supports our work – our research has the potential to save thousands of lives. You make this possible, thank you.
---
You may also be interested in:
Join us for the launch of the Nottingham Breast Cancer Research Centre
Discover more about our exciting plans for our new breast cancer research centre, hear talks from patients and researchers and go behind-the-scenes with laboratory tours.
The people behind the papers
Meet six researchers who work tirelessly behind the scenes to create a brighter future for children with brain tumours.
Living with 'scanxiety'
In the four years that he lived with a brain tumour, Sam White endured more than 25 distressing scans. His parents Mike and Pam, share how Sam's experience has helped transform the process for other children.