Progress on the High Dependency Unit (HDU)
's care is handed over to the critical care staff. On arrival, she is pale and aware of her surroundings.
Current treatment and care: Blood gas shows metabolic acidosis. Results of all previously taken blood tests need to be analysed. Any blood tests that are outstanding need to be taken. Ensure 2 sets of blood cultures (as per local policy) are taken, further FBC, urea and electrolytes and CRP levels are checked.
Ongoing progress overnight: Metabolic acidosis continues.
Current treatment and care: 1.8 mmol/L. Where the lactate level remains high, further fluid resuscitation will need to continue.
Ongoing progress overnight: Lactate was checked at 04:00 and had increased to 2.2 mmol/L, necessitating further fluid bolus.
Current treatment and care: Chest x-ray taken which shows a white patch in the right lung suggesting consolidation and pneumonia. Tazocin was initially given thinking had a UTI which was the source of her sepsis. However antibiotics are changed to target the community acquired pneumonia and initial intravenous doses are given. Urine specimen is sent (23:30) to test for pneumococcal and legionella organisms.
Ongoing progress overnight: New antibiotics prescribed continued. No new results received overnight.
Current treatment and care: Vasoactive medication, via a central line, is started to support the hypotension. Noradrenaline infusion is commenced with the effect of increasing the SBP to 94 mmHg. An accurate urine output needs to be assessed. Catheterisation (21:40) reveals a residual urine of 50 mL. Hourly urine output monitoring is started. The aim is to ensure a minimum of ½ mL per kg body weight is produced hourly. This indicates that the patient is well perfused and the kidneys are working efficiently. For (weight = 63 kg), a volume of at least 30 mL/hr urine is expected.
Ongoing progress overnight: Noradrenaline infusion is increased to 10 mL/hr to maintain SBP > 90 mmHg. A further fluid bolus is given overnight in response to the lactate level rise. Hourly urine output measurements remain minimal throughout the night.
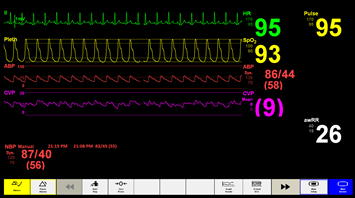
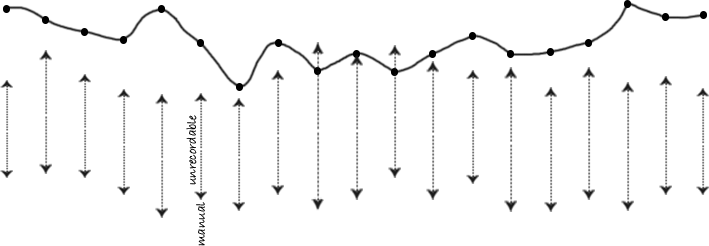
Current treatment and care: Oxygen therapy continues at FiO2 40% to maintain SaO2 at 94%. Initially on HDU, her BP is unrecordable on the Dinamap. However a manual check reveals her BP has fallen to 88/40 with a tachycardia of 110 bpm. The severity of the situation for means she requires continuous monitoring in a critical care area to provide the means to detect potential problems occurring earlier. Arterial and central venous pressure (CVP) lines are sited.
Ongoing progress overnight: BP remained low. CVP was variable, between 7 and 10 mmHg, responding to the fluid bolus given at 04:15. The noradrenaline infusion initially improved the BP, however the infusion was gradually increased as the response was not maintained.
Current review: 's care will need reviewing overnight if her condition deteriorates or on the morning ward round.
Overnight: Multiple fluid boluses have been given maintaining CVP but with a minimal urine output and fluctuating BP. A continuous noradrenaline infusion was started, with some effect. The morning ward round will need to consider the possibility of transferring to the Intensive Care Unit (ICU) for further vasopressor medication and potentially inotropes (e.g. dobutamine or adrenaline).


 )
)