Previous blog posts
All the blogs we've posted are eventually moved to this archive page.
Eczema Care Online - One Year On...
It’s now been over a year since we first launched the Eczema Care Online website (www.EczemaCareOnline.org.uk). We thought it was time we gave you an update on how things are going.
The Eczema Care Online website has been accessed by over 20,000 people from 157 countries around the world. This is an amazing achievement, but with millions of people living with eczema in the UK alone, there is clearly a long way to go.
Here are some of the things that people have been saying about Eczema Care Online:
I thought I knew how to look after my child’s eczema, but I learned so many new things from ECO about how to keep eczema under control – things I would have never thought of!
Study participant, parent of a child with eczema
It was one of the best websites I’ve ever used; it was really easy to use and provided the answers to your specific questions. I didn’t have to read through lots of stuff that wasn’t relevant to me.
Study participant, young person with eczema
Very helpful resources indeed. Since it has become available, I have tried to include it in every Advice & Guidance that I do!
Paediatric Dermatologist, UK
Looked brilliant because you can just send it away to [patients] and say look, this is what it’s all about
General Practitioner, UK
Our Family Workers regularly signpost families to ECO so hopefully there is a steady stream of families benefiting from the information.
Eczema Outreach Support, UK
Our two randomised controlled trials showed that Eczema Care Online improved eczema symptoms. It also helped people to cope better with their eczema. You can read the full trial results in the British Medical Journal. Or you might prefer to watch our video (link to video).
Our aim is to make sure that the website is available to everyone with eczema. Ideally, healthcare providers will signpost to the website whenever someone asks about eczema. We would love it if all primary care staff, including GPs, health visitors and pharmacists were aware of Eczema Care Online. We hope they will prescribe it alongside eczema treatments. We’ve made this easy by adding a link to Eczema Care Online within primary care electronic health systems (via the Ardens template for eczema).
We are also delighted that Eczema Care Online is mentioned in key national guidelines such as:
- NICE Guidelines for children with eczema (web link)
- Clinical Knowledge Summaries (weblink).
Key supporters include the British Association of Dermatologist, British Dermatology Nursing Group, Primary Care Dermatology Society, and of course the wonderful National Eczema Society and Eczema Outreach Support charities.
You can read an article about Eczema Care Online that was published in the National Eczema Society’s Exchange magazine (link to pdf of article).
We need your help.....
Can you help us to spread the word about Eczema Care Online?
When it comes to sharing good news, there is nothing quite like word of mouth. If you know someone with eczema, please do share.
Website: www.EczemaCareOnline.org.uk


Eczema Care Online Toolkits available
by Miriam and Ingrid
We are delighted to share with you that the Eczema Care Online toolkits for parents/carers of children with eczema and for young people with eczema are available at EczemaCareOnline.org.uk.
This is not the completely finalised version – we are still completing the Welsh translation and some details so please tell us if any features of the website are not working by emailing eco@soton.ac.uk.
We hope that you will all share the link to the toolkits widely; we will be working over the next year to encourage doctors, nurses and pharmacists to signpost people with eczema to the toolkits.
Please do share the EczemaCareOnline.org.uk link with anyone who you think might be interested or who might find the toolkit useful. We have had fantastic feedback from users so far. One parent of a child with eczema said:
“It was one of the best websites I’ve ever used; it was really easy to use and provided the answers to your specific questions. I didn’t have to read through lots of stuff that wasn’t relevant to me.”
One of the teenagers who used the website said:
“It’s great if I have a quick question about something. Before I would have harassed my mum to take me to the doctors, which is a pain if you just have a very basic question, but now I just have a look on the website.”
We would like to thank all the people who took part in this research, particularly the young people and families living with eczema.
June 2022


Cochrane review on the best and safest ways of using topical corticosteroids now published
by Steph & Jane
We have now published a Cochrane systematic review on the best and safest ways of using topical corticosteroids – this large review includes over 100 research studies looking at different ways of using topical corticosteroids for eczema. The studies evaluate the safety and effectiveness of different strengths of steroids, how often to apply the steroids, how long to apply them for and how best to prevent eczema flares. Further information about our publications and outputs can be found on our publications page.
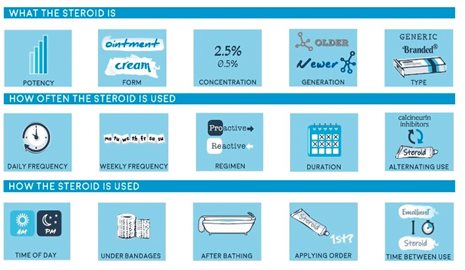
A summary of the key findings from the review:

We have used the information from this review, and from our interviews with people with eczema when developing the Eczema Care Online Toolkit, to produce guidance on how to use eczema treatments in the safest and most effective way.
Some of the resources available include:
Two treatments used well: A guide for eczema self-care.
Guidance on how to choose between different moisturisers:

This decision aid is designed to be used by parents, older children with eczema or health care professionals.
It was developed by researchers in collaboration with stakeholders, and is based on the finding from the Best Emollients for Eczema trial, which evaluated the effectiveness and acceptability of lotions, creams, gels and ointments that are commonly prescribed on the NHS.
January 2022

Looking forward to 2022 - an exciting year for the Eczema Care Online Programme
by Kim
The coming year is all set to be an exciting time for the Eczema Care Online team and for all those who have contributed, supported, and encouraged our efforts over the last few years.
Here are some highlights of things coming up soon for you to look forward to:
Eczema Care Online Toolkit soon available for use – we have been working with an external web design company to develop a user friendly webapp that will allow people to access the Eczema Care Online Toolkit for the first time outside of a research setting.
The eczema Care Online Toolkit provides a one-stop shop for easily digestible information about eczema, how best to use eczema treatments and a host of other information about living with eczema, such as how to avoid triggers, manage stress and how to make the most of GP consultations.
As part of this we have produced some engaging videos that you might like to share with others:
Eczema Care Online Trial results coming soon – results of two randomised controlled trials using the Eczema Care Online Toolkit will be available later in 2022. These trials have tested two slightly different versions of the toolkit; one aimed at parents or carers of children with eczema, and another version of the toolkit designed to support young people with eczema as they start to manage their eczema for themselves.
These clinical trials have included almost 700 participants and have followed people up for 12 months to see whether or not people are better able to manage their eczema after having used the toolkit.
Cochrane Systematic on the best and safest ways of using topical corticosteroids – this large review has just been accepted for publication and will be available soon. It includes over 100 research studies looking at different ways of using topical corticosteroids for eczema. This includes studies evaluating the safety and effectiveness of different strengths of steroids, how often to apply the steroids, how long to apply them for and how best to prevent eczema flares. Look out for our next blog which will outline findings from this review. For further information about our publications and outputs can be found on our publications page.
October 2021

Stakeholder workshops on key messages about the safety and effectiveness of topical corticosteroids
by Paul
In our January blog Kim and Miriam reported that the ECO team had almost completed the Cochrane systematic review on the safety and effectiveness of topical corticosteroids, the most commonly used flare control cream. To help the findings reach a wide audience the team have started to distil a small number of ‘key messages’ for families with eczema and for health professionals. These key messages bring together the best research evidence from the review with current guidelines about how to manage eczema.
To test these key messages, we hosted a series of workshops for people with eczema, parents of children with eczema, and with different health professionals (including pharmacists and GPs as well as dermatology specialists). We also hosted a workshop with people who are concerned about use of flare control creams. In total 38 people attended our online workshops. We asked them about their views on the messages and how we could make them more useful.
People who attended the workshops welcomed having key messages to clarify the safest and most effective way to use flare control creams. People living with eczema in particular told us that different information from different sources can be confusing, and that a single source of consistent information (such as our research review) would be very helpful.
Short messages were generally considered to be more user-friendly and less likely to be off-putting to people. Health professionals also liked simple messages but thought that providing more detailed summaries alongside the key messages could be useful for those that wanted more information.
People felt that the key messages about flare control creams, and the insight gained in the review, might be most effective when integrated into a more all-encompassing eczema management package. Different groups recognised different ways in which this might be done to support people with eczema, GPs, pharmacists, or the parents of children with eczema. This is our next challenge! Developing resources to deliver the key messages and identifying avenues that will reach the different groups in a way which is useful and practical to them.
We have taken all the feedback on board and are now refining the key messages to add clarity and meet the needs of families with eczema and health professionals. We look forward to sharing them with you soon!
Why did we do this research?
Adolescence and early adulthood can be a particularly challenging time, especially for young people with eczema. When they were younger, their families mainly looked after their eczema, but now they have new roles and responsibilities around their eczema. More research is needed to better understand the specific challenges that this group face when looking after their eczema.
What did this research look at?
Our research wanted to find out about young people’s experiences of looking after their eczema and their interactions with health professionals. We spoke to 28 young people aged 13-25 years. The audio from each interview was written up and the authors looked for patterns in the data.
What did we find?
Generally, young people felt that their prescribed treatments helped their eczema. However, some young people were not convinced that their treatments helped in the long-term and some were worried about the safety of their treatments. Young people welcomed the opportunity to be more involved in looking after their eczema, but talking to health professionals, getting prescriptions, or moving to an adult clinic, could sometimes be daunting. Young people were more likely to avoid doing things that made their eczema worse if they personally believed that doing so would help their eczema. However, it was not always easy to avoid everything that made their eczema worse. For example, young people found it hard not to scratch and some triggers, such as the weather, were hard to avoid.
What did we recommend from this research?
Our research paper recommended that healthcare services should encourage young people to discuss their needs and treatment concerns with health professionals. Young people should also be given the skills and confidence to look after their eczema and talk to health professionals. As part of the ECO project, we used these research findings to help us to create the online toolkit for young people with eczema. Specifically, it helped us to make sure the information and support provided in the toolkit met the needs, and addressed the concerns, of this group.
The full paper is available to read online.
The ECO trials finished recruiting enough volunteers in December 2020 in order to find out whether the ECO toolkits make a difference to people in managing their eczema. Thanks to the help of the GP practices, parents of children with eczema and young people with eczema, there are now 677 people in the trials; 340 parents of young children with eczema and 337 teenagers and young adults. As part of the trial we ask participants to complete questionnaires for a whole year. This seems like a long time but eczema can vary a lot over a year, so we need to make these comparisons over this time to make sure we get the right result from the research. We look forward to being able to share the results of the trials in 2022.
The other exciting news is that we have nearly completed the Cochrane systematic review on the safety and effectiveness of different strategies for controlling eczema using flare control creams (commonly topical corticosteroids). Cochrane reviews are the gold standard for pulling together the results from lots of different research. We hope to be able to share the results of this as widely as possible in 2021.
Watch this space! Or get in touch via ECO@soton.ac.uk if you would like to take part in stakeholder workshops. We are keen to talk to people and families with eczema and healthcare professionals, including pharmacists, to understand how to share the key findings from this research in ways that are meaningful and helpful.
When people think of eczema, they usually only think of what we can see – the skin changes and scratching. But there is more beyond the skin; pain, itch and lack of sleep that have a huge impact on people’s lives. To be able to develop resources that are relevant to young people with eczema we wanted to know what their psychosocial needs were when dealing with both visible and invisible eczema symptoms. This paper, “Psychosocial needs of adolescents and young adults with eczema: a secondary analysis of qualitative data to inform a behaviour change intervention” has been published in the British Journal of Health Psychology.
We looked at interviews with 28 young people aged 13 to 25 with experience of eczema. They said they had mixed feelings about the visibility of their eczema. On one hand they didn’t want other people to see their eczema or to stand out because of their skin but on the other hand they wanted others to understand that the eczema has a major impact on their lives when it’s bad. Young people often felt self-conscious, for instance when they have to deal with advice, they did not ask for from people suggesting how they should look after their eczema.
When young people met others with eczema and saw that they were not alone with this condition they were more likely to want others to understand their experiences. The young people we spoke to were keen to show that eczema comes in all shapes and forms, can be mild and can be severe, can be gone and can come back. Our new paper can bring more awareness to the complexity of the condition and managing both visible and invisible symptoms.
Importantly, such complexities also led to a need for emotional support from health care providers, from peers with similar experiences and from online resources. Here at ECO, we are testing the online resources that we developed to be able to provide support that adolescents and young adults are seeking.
To read the paper it is available here:
Ghio, D., Greenwell, K., Muller, I., Roberts, A., McNiven, A., & Santer, M. (2020) Psychosocial needs of adolescents and young adults with eczema: A secondary analysis of qualitative data to inform a behaviour change intervention. British Journal of Health Psychology DOI: 10.1111/bjhp.12467
If you are interested in our other work with young people with eczema:
Ghio, D., Muller, I., Greenwell, K., Roberts, A., McNiven, A., Langan, S. M., & Santer, M. (2019). “It’s like the bad guy in a movie who just doesn’t die”: A qualitative exploration of young people’s adaptation to eczema and implications for self-care. British Journal of Dermatology. DOI: 10.1111/bjd.18046
What are children’s thoughts and experience of eczema? Lots of studies have explored this in young people and parents, but very few studies so far have looked at how children experience living with eczema. As part of the ECO project we were keen to find out about eczema from children’s perspectives, so we interviewed 14 children aged 6-12 years old about their views and experiences of eczema and eczema treatments. This was such a fun, rewarding and insightful experience! To help the children feel at ease and feel able to share their experiences with us, we used a range of age-appropriate techniques that we would like to share with you in this blog.
Interviewing children can be challenging so we wanted to make sure we did everything we could to help them feel comfortable during the interview. We adopted a chatty conversational style and used a set of open-ended questions to help guide the interviews. We made sure that questions were phrased in child-friendly language and tried to focus on the child’s interests (Docherty and Sandelowski 1999, Madden, Shilling et al. 2016). After explaining the purpose of the interview and checking that they were happy to talk to us about their eczema, we asked the children about their interests and favourite activities. This usually prompted them to show us their favourite toys, books, stories they had written, pictures they had drawn, artwork they had made and certificates or awards they had won. We found this was a lovely way to start to the interviews and to build rapport with the children!
During the interviews we used lots of creative and fun activities such as picture cards related to the interview questions to guide the conversation and engaging play activities (Clark and Moss 2011, Kellett 2011). Following an initial chat about the child’s favourite activity, we introduced them to a whale toy (based on the ECO study mascot), colouring pencil set and ECO whale drawing and colouring sheets, as well as stickers (various shapes and colours) and Lego bricks. We wanted to assume the ‘least adult role’ to encourage active participation in the interview (Mandell 1988). We did this by sitting on the floor with the child and engaging in their chosen activities (e.g. helping build Lego, choosing stickers or colouring pencils), and allowing the children to ‘direct the research agenda’ by choosing to use pictures cards or to express their views by drawing their responses to some questions. By using these techniques, we hope that the interviews were a rewarding experience for all involved and they certainly provided us with valuable insights into children’s perspectives of eczema and eczema treatments.
We are writing a paper all about what children told us about their eczema, which we will post on the website as soon as it is ready. We will produce a summary for children as well as a summary for their parents and carers.
Clark, A. and P. Moss (2011). Listening to young children: The mosaic approach, Jessica Kingsley Publishers. Docherty, S. and M. Sandelowski (1999). "Focus on qualitative methods: Interviewing children." Research in nursing & health 22(2): 177-185.
Kellett, M. (2011). "Empowering children and young people as researchers: Overcoming barriers and building capacity." Child indicators research 4(2): 205-219.
Madden, L., et al. (2016). "Questioning assent: how are children's views included as families make decisions about clinical trials?" Child: care, health and development 42(6): 900-908.
Mandell, N. (1988). "The least-adult role in studying children." Journal of contemporary ethnography 16(4): 433-467.
The ECO study has reopened to new recruits. We are very grateful to practices, parents of children with eczema and young people with eczema for making this possible. We have already recruited 98 people since reopening the study, bringing the total to 259, which is fantastic and puts us in a great position to meet our recruitment target.
The GPs and Dermatology Teams working on ECO are getting used to providing care via telephone and video consultations, sometimes supplemented by photos and face-to-face (with masks) where really necessary. So we would encourage people who are struggling with their eczema to get in contact with health services if they need a prescription for more treatment or are struggling to get control of the eczema themselves. We wrote about handwashing in our last blog, but this has been such a big issue for people with eczema during covid that we would like to mention again. Consultant Dermatologist Professor Hywel Williams has made a fantastic video about hand washing and eczema.
In summary:
• Follow NHS advice on how and when to wash hands
• You or your child can use soap and water to wash so long as you put plenty of emollient (moisturiser) on afterwards to keep the skin healthy.
• If you have to go out, make sure to take emollient (moisturiser) so you can apply it after washing or if you have to use a hand sanitiser. Use a pump dispenser or tube for the emollient to avoid spreading germs.
We are really grateful to everyone who has signed up to the ECO study so far. More than 150 people are taking part and continue to complete their questionnaires, even during these uncertain times. We are not inviting new people into the study at the moment. This is because people are invited through their GP surgery and we don’t want to add to their administrative work at this time. For those already in the study, follow-up questionnaires are going as planned and the website remains open to support people. We plan to reopen the study to new participants as soon as possible.
The world may be different when covid has passed, but two things are certain: (1) eczema will still have impact on many people’s lives and (2) providing high quality support to help people to manage eczema will be as important as ever. We remain committed to answering the research question about how best to provide this support.
Many of us working on ECO are health professionals and are aware that people are being careful not to contact the NHS at this time. Although services have changed (more telephone and video consultations), we would urge people who are struggling with their eczema to get in contact with health services if they are unable to get control of it themselves.
Finally, a lot of people have asked about handwashing in eczema. ECO contributor Professor Hywel Williams has made a fantastic video explaining this here https://mediaspace.nottingham.ac.uk/media/COVID-19+hand+washing+advice/1_wlufymil
Simple summary:
- Follow NHS advice on how and when to wash hands here https://www.nhs.uk/live-well/healthy-body/best-way-to-wash-your-hands/
- You or your child can use soap and water to wash so long as you put plenty of emollient (moisturiser) on afterwards to keep the skin healthy.
- If you have to go out, make sure to take emollient (moisturiser) so you can apply it after washing or if you have to use a hand sanitiser. Use a pump dispenser or tube for the emollient to avoid spreading germs.
This content of this blog post was written for, and first appeared on, the BMJ website.
Amina Ahmed and Carron Layfield discuss how they set up a collaborative initiative at the Centre of Evidence Based Dermatology in Nottingham and what it’s achieved
Amina Ahmed: The patient panel members perspective
Eczema treatment I’m a full-time working mother of three children between the ages of 7 and 16 years old, two of whom have had severe eczema since the age of 3 months. This has presented us with difficult life and career choices and we have struggled to cope with the condition at times. When we realised there was no miracle cure it was heart-breaking, but the biggest frustration was dealing with health professionals who held very different views on best management. I joined the Centre of Evidence Based Dermatology’s (CEBD) patient panel ten years ago and it opened my eyes to how disjointed research is and the patchy nature of clinical evidence in dermatology. My hope has been that participation in the panel may play a small part in promoting research into questions which reflect the realities of people’s lives and how they cope with skin conditions. As a parent it’s been particularly important to me to speak out about how severe eczema can result in children being denied the simple pleasures in life, such as walking barefoot on a beach or going swimming; and to promote researchers understanding of how eczema affects children emotionally, physically, and mentally. Being on the panel has provided a safe and supportive environment to ask simple questions, and though I don’t always understand all the technical jargon around research I know I can always reach out to other members of the panel or its co-ordinator for clarity and discussion of my role as a panel member. Since joining the panel I have been a co-applicant for clinical trials, acted as a patient/carer reviewer of research studies, reviewed patient leaflets, sat on research steering committees, and been interviewed for radio and newspapers. I have also participated in a James Lind Alliance Priority Setting Partnership in 2011. [1] To ensure members were clear on the support that researchers were seeking I also helped create study templates for researchers to produce lay summaries of their work and guidance for patients who participate in research. As the work of the CEBD covers a wide range of skin conditions I invited other panel members to share their experiences alongside mine.
Peter Smart: I have been actively involved as a participant in a research study on cellulitis, a condition I have had repeatedly suffered from. I have also reviewed several draft protocols for studies and commented from a consumer perspective on reports prior to publication, mainly on systematic research into cellulitis but also necrotising fasciitis. I have also been a patient co-author and named contributor of a number of published papers (5,6) and I was a member of the CEBD Priority Setting Partnership on cellulitis. [2] In 2018, I also contributed to the #PatientsIncluded discussions at the Cochrane’s global Colloquium in Edinburgh and reviewed twenty abstracts ahead of the meeting. My stipend for attending the meeting was paid by the organisers
Carolyn Hughes: I have been affected by psoriasis and psoriatic arthritis and joined the panel to help other people. My first panel meeting inspired me to get involved with Cochrane Skin and as a patient I have commented on several Cochrane reviews over the past 10 years. I’m now a Cochrane author and have written plain language summaries for four Cochrane reviews of treatments for psoriasis. Most recently I was involved in the James Lind Alliance’s Priority Setting Partnership to identify research priorities in psoriasis
Carron Layfield: Co-ordinator of the patient panel
I am a research manager by background and have worked at the Centre of Evidence Based Dermatology (CEBD) in Nottingham for twelve years. The centre has long involved patients and carers in research, but many indicated they would value a long term partnership with the unit and the chance to undertake training in research methods. In response we set up a Patient Panel in 2009 to provide a more supportive, and sustained link with patients and carers, which we believed, would also increase the quality and clinical usefulness of our research to the patient community. As the centre undertakes paediatric research we included both patients and carers ( mostly parents) and we get input on an on-going basis from our local Nottingham Young Persons Advisory Group when direct involvement from children and young people is needed.
We invited patients and carers who had previously worked with us to join the panel and put out a call for interest to patient organisations including The National Eczema Society, The Psoriasis Association, the Vitiligo Society; wider patient involvement groups such as People in Research and through the CEBD website. The sole criteria was experience of living with a skin condition, or looking after people who have them. Within six months we had established a panel of 20 patients and carers from across the UK affected by a range of skin conditions. Since November 2009 we have held regular (usually) annual meetings, where speakers include patients and carers and have run training courses on research methods, including Cochrane systematic reviews, and evidence based medicine, and jointly discussed what makes a good and bad clinical trial, and the importance of jargon busting as part of these. We also encourage panel members to attend the conferences that the centre runs, participate in relevant Cochrane meetings and take advantage of the opportunity to take on-line training courses in PPI such as the one established by INVOLVE.
We now have 30 panel members who communicate with us regularly via e mail and Panel members have been involved in CEBD research in a wide variety of ways as set out above. We aim to maximise opportunities for involvement of panel members and so contact them on an on-going basis about projects and we have developed templates with the panel to facilitate this exchange. It’s been very helpful to have a cohort of patients and carers who we can readily reach for timely input. Maintaining regular contact with a group that meets only once a year is vital and we circulate newsletters on a quarterly basis; these include updates on studies, relevant training opportunities and “meet a member” articles authored by panel members outlining their experiences. Another crucial aspect of retaining engagement is providing timely and meaningful feedback to those who have provided input into projects.
The CEBD patient panel has also influenced work beyond research at the Centre. The Nottingham Eczema Support Group for Carers of Children with Eczema for example is run by a panel member (Amanda Roberts), allowing new research knowledge to become integrated quickly into patient information leaflets that in turn promote better evidence-based patient care. Other members have become engaged with working as expert PPI members for organisations such as the NIHR.
The challenges of establishing and maintaining a patient panel include managing expectations of both researchers and panel members. We have found that researchers can have a tendency to leave things until the last minute and want very rapid feedback from patients. It’s also essential to remember that we are sometimes asking patients to share very personal information and this can be hard to do. Sensitivity is important. With patients we have found that they sometimes want to volunteer for more than they can readily take on, and can initially have unrealistic expectations of timelines for research projects and how soon findings may make a difference to patients lives. When people first get involved there can also, quite understandably, be a lack of awareness of the difficulty and complexity of getting funding for research projects.
To maintain a constructive dialogue between patients, carers and researchers at the Centre (and undertake all the related administration and organisation) it has been critical to have a panel co-ordinator. Currently the time I devote to the panel is around 5 hours a week. The cost of our annual panel meeting and training events is around £2,500 taking into account travel and accommodation costs, venue costs, and catering. Such costs are included as PPI training costs in relevant grant applications. Given inevitably limited resources we are very fortunate that panel members are often happy to contribute their time and expertise on a voluntary basis for projects that are not yet funded.
The CEBD Patient Panel has undoubtedly had a positive impact on CEBD research and it has been great fun working together. We are currently reviewing our activities against the new UK public involvement standards for research. Future plans for joint working include a mentoring scheme for new panel members and a stronger focus on co production of research.
© BMJ Publishing Group Limited 2019.
For references, please see the original version on the BMJ's website. Many thanks to the BMJ for giving us permission to include this content.
October 2019 - Diverging views on eczema treatments

Miriam Santer

Amanda Roberts
This content of this blog post was written for, and first appeared on, the BMJ website.
Recent years have seen increasingly polarised and acrimonious debate about the role of topical corticosteroids in the treatment of eczema. On one side are patients and parents who decline a treatment they believe to be addictive or toxic. On the other are health professionals troubled by what they see as harmful refusal of an effective treatment. In some cases, parents have undergone child protection investigations as a result of declining treatment with topical corticosteroids. Important influencers in the debate include patient organisations, the pharmaceutical industry, and both social and mainstream media
Language in this area has become emotive and contested, contributing to mistrust and misunderstanding. Health professionals have written about “topical steroid phobia” and “treatment refusal” while patient groups feel this is a dismissal of their legitimate concerns. [1] Some patient groups wish for greater recognition of “topical steroid addiction,” whereas medical consensus is that “red skin syndrome” is a consequence of rare over-use, not the result of a common addiction. [2,3] Such different perspectives have major consequences for people with eczema, particularly children.
Parents of children with a visible condition, such as eczema, are used to strangers offering well-meaning but often conflicting advice. This, in addition to conflicting advice from health professionals, can lead parents to seek resolution online. [5] Many choose online discussion forums where narratives are often polarised and combative, leading to further bewilderment and confusion. [6]
A divergence in views on eczema treatments is also apparent among different patient groups. Evidence based guidance recommends intermittent topical corticosteroids for children with eczema, with only a very limited role for antibiotics. [7] But a brief online search using the terms “my child has eczema” reveals the overwhelming popularity of two polar opposites: (i) products combing a topical steroid and a topical antibiotic, obtained privately on line, and (ii) rejection of the use of topical corticosteroids altogether. [8,2]
While the websites of mainstream patient organisations often give traditional evidence-based or consensus-based advice, their linked Twitter or Facebook groups can become polarised, angry, and alarming places for new users. Many organisations struggle to provide their patient group with a balanced collective “voice.”
Further complications arise when organisations are part funded by the pharmaceutical industry. [9] Commercial actors tend to focus their attention on a small number of patient organisations, carefully selected for their “advocacy potential.” [9] Pharmaceutical company funding is particularly problematic when industry interests align with popular opinion. The existence of topical steroid “addiction,” for example, aligns well with the interests of companies developing alternative treatments for eczema such as biologics. [10]
Effective management of long-term conditions can be heart-breakingly difficult for patients and carers, but also challenging for health professionals in the absence of a shared understanding about treatments. Health professionals may feel that they don’t have the time or resources to “turn” what they view as an unsubstantiated idea. Some have called for “better evidence, better presented, better explained, and applied in a more personalised way,” in order to help patients and carers use the same evidence-base as health professionals when making decisions about treatments. [11] Others emphasise that shared understanding requires more than just readily usable patient summaries. Health professionals need the right tools and the skills to engage in dialogue, but they also need the right attitude.
Further research to identify the most effective resources for promoting shared understanding would benefit everyone, including moderators of online discussion forums, who play an important role and need more support in highly polarised contexts such as use of topical corticosteroids for eczema. [13]
Health professionals may find it easier to engage in dialogue around treatment controversies if they have a greater awareness of the online background that patients or carers bring to the consultation. As well as fostering these skills and attitudes in undergraduate and postgraduate curriculums, professionals could invest time exploring exchanges on platforms such as Facebook, Mumsnet, or Student Room. Even brief sessions could improve understanding of patient concerns in disputed therapeutic areas. Ideally, health professionals would have access to a social media “digest” similar to digests available through mainstream media.
Finally, the lack of transparency around industry funding of patient organisations is a barrier to resolving highly polarised debates about treatments. Greater transparency would help both patients and health professionals identify information that could be biased by commercial interests.
For references, please see the original version on the BMJ's website. Many thanks to the BMJ for giving us permission to include this content.

Julie Hooper
Introduction
Ever wondered what our Trial Manager, Julie does? Here she tells us in her own words.
What will I do?
Working within a fantastic study team who have worked so hard to design and test the online eczema toolkit, we are now preparing to go live! This is the exciting phase of our study where we ask young people and families of children with eczema to sign up to the study and use our online toolkit to see if it can help them manage their eczema more effectively.
My role is demanding, exciting, and a role I am extremely passionate about. It involves juggling many different tasks at the same time, with many deadlines and protocols to adhere to, whilst ensuring that the families and young people taking part are treated with the utmost respect, their expectations are managed well, and they have a good experience of taking part in research studies. I will also get to meet many lovely people all across the country who are keen to help make this study a great success.
Our regular planning meetings with dedicated research teams give us the best opportunity possible to deliver a successful trial with positive results for young people and families with eczema now and in the future. Patient & Public Involvement (PPI) representatives willingly share with us their eczema expertise from a public perspective. GP surgeries across the South of England, West of England and East Midlands will be helping us recruit patients with eczema. Our GP practices are brilliant at supporting and helping us run research studies. We appreciate how very busy they are so these processes can take a lot longer to complete than people might think so patience, regular communication and good planning is the key!
Managing the ECO study
We are planning to work with 80 GP practices to recruit 400 people who have eczema between October 2019 and June 2021. The study will include children and young adults up to the age of 25 years. Practices will invite suitable patients by invitation letter to take part if they wish. They will stay in the study for a year and complete questionnaires online over this period so we can measure the difference in self-reported eczema severity.
These questionnaires are extremely important to the outcome of our study so a high completion rate is essential in helping us to judge whether the ECO toolkit has helped people with eczema or not, so it is important that participants complete as many of the questionnaires as possible. 200 people will have access to our online toolkit where they will have access to hints and tips about eczema straight away. The remaining 200 will be offered access at the end of their participation in the study.
Looking to the future – what outcome are we hoping for?
If websites that support people to manage their eczema more effectively are proven to be helpful, it is the ECO study team’s hope that health professionals will ‘prescribe’ these as part of routine NHS care.
Taheeya Ahmed
As a first-year college student dealing with eczema for almost 17 years now hasn’t been the easiest however I am slowly starting to find my way around it. Like many others, I have had eczema for as long as I can remember and during primary school, I always used to see it as a hindrance and embarrassing to be the only one with dried up, flaking and bleeding hands. As I started secondary school, my eczema really affected my self-esteem. Knowing I would have to meet all these new people, make new friends and watch them silently judge and stare at my hands was horrible. However, as I got older and began to explain the condition to my peers and friends, things began to become easier and I began to find my confidence again. I stopped letting my eczema get in the way and to some extent, using it as an excuse to shy away from certain situations. These days my friends will remind me to put some cream on, if they notice my hands are dry and it’s amazing to see how things have changed over the years.
Since being part of ECO, I have learnt new things about eczema that I previously hadn’t known, even though I’ve had it for ages, and it has further strengthened my interest to study medicine. The website will be extremely beneficial for young people living with eczema and it has been so well thought through and the concepts are well portrayed. I am really excited to see the website progress further and pleased to have been a part of the project so far.
It’s time to debunk a myth about eczema.
Eczema is not ‘just’ a childhood condition.
For some young people, they continue experiencing symptoms of eczema as they grow older and these symptoms change over time. Our paper exploring what it is like for young people in their late teens/early 20s to have eczema has been published in the British Journal of Dermatology. Our paper is titled: “It’s like the bad guy in a movie who just doesn’t die”: A qualitative exploration of young people’s adaptation to eczema and implications for self-care. The quote itself is from a young person describing her eczema. Through her description and those of other young people we found that, for them, eczema keeps coming back over their lifespan. This we called the ‘episodic nature’ of eczema and we found that it has implications and poses challenges for how young people deal with eczema physically and mentally - challenges we felt should be acknowledged to help identify how best we can support young people in managing their eczema.
We picked the quote for the title because we felt it captures a struggle that a lot of young people discussed and how it can feel like when managing eczema. That it can be like a battle scene in a movie that does not end. But the point perhaps is not to kill it, the eczema in this scenario, but learning to live in peace together.
What did this mean for our research programme?
The Eczema Care Online (ECO) project is developing toolkits to promote self-care. Self-care for us means those people dealing with eczema working together with health professionals to find ways that work best to keep eczema under control. We have listened to those challenges that young people face and have worked together with them to develop toolkits that can provide that support when struggling with eczema. We used a process to develop these toolkits, known as the Person-Based Approach in which identifying challenges and how to overcome them is a key part of the process.
What’s next?
We have been busy collating all the information and expertise in our wider ECO team and testing the prototypes of the toolkits we developed. Watch this space as we continue to update you on the progress of the research programme!
Sandra Lawton OBE
MSc, RN, OND, RN Diploma (Child) ENB 393 Nurse
Consultant Dermatology, Queen's Nurse
Rotherham NHS Foundation Trust
Working in dermatology for over 30 years I feel well placed to sell dermatology nursing to the world and the contribution nurses make to patients and their families. We commonly hear graphic descriptions from patients and their families describing their experiences, battles to be heard and to see a specialist with the many myths and uncertainties around their eczema or that of their children or family member often dismissed as unimportant. There is no doubt nurses develop a special bond with their patients and families. Skilful and compassionate nursing can provide great relief for our patients who want to feel “feel safe, secure, accepted and informed” about their eczema and have the confidence to deal with it on a daily basis. This was our nursing philosophy in Nottingham and one I have aspired to throughout my dermatology career.
Information sources for our patients often start at home with friends and family-giving advice based on hearsay and no sound evidence. Added to this parents frequently recount stories of people coming up to them in supermarkets or the street and saying “Oh have they got eczema have you tried? >>>>>>>” Social media and the internet also provide challenges with reliable sources of information competing with a wealth of dodgy sites which have the potential to confuse and scare patients and their families about eczema and the products used to treat eczema.
This is where nurses have an important role to play in the patient’s eczema journey, they have time to listen, unpick, and dispel myths and signpost families to high quality information relevant to their discussions. Having developed and worked within a children’s eczema clinic for over 20 years listening is an issue for many of our children and their families who feel their voices and stories are not heard and comments such as “Its only eczema, they will grow out of it” are not helpful and upsetting for children and their families. In addition nurses can provide practical realistic advice about when and how to use treatments. In clinics we frequently see long lists or carrier bags full of products, prescribed or purchased for eczema but nurses can help to simplify things in order to make eczema care achievable. I have used the analogy of cooking previously when describing realistic plans for patients and their families with eczema: You can provide several ingredients and the outcome is likely to be successful or you can provide a huge ingredient list which will potentially lead to failure. The key is to work with and listen to our patients and their families by keeping it simple with two treatments. So moving forward ECO (Eczema Care Online) aims to help parents, children, and young people “get control and keep control of their eczema”. ECO will never be a replacement for an eczema consultation but will be a welcome additional resource for patients and families looking for reliable accessible information and realistic eczema plans.
People with eczema and their parents /carers have told us they are worried about conflicting advice they have received from different health professionals about what is ‘safe’ use of topical steroids. In ECO we are pulling together all the available evidence on topical steroid safety in a way that will make it easier for everyone to understand, including people with eczema, their parents, carers and healthcare professionals.
Cochrane systematic review of randomised controlled trials
Our main review is a Cochrane systematic review that will explore the best and safest ways of using topical steroids, based on evidence from randomised controlled trials. This review will help people to understand the likely benefits and harms of using topical steroids to manage eczema. For example, someone with eczema might be thinking about how often to apply their topical steroids - should it be once a day or twice a day? In our review, we will pull together all of the available clinical trial data to look at whether applying topical steroids once a day is as good as twice a day and whether using topical steroids once a day lowers the chances of side-effects. By working to Cochrane standards we will ensure that we produce a high quality systematic review.
Review of long-term studies of topical steroid safety
Although randomised controlled trials are the ‘gold standard’ of evidence, they often only look at quite short-term effects and are not ideal for picking up longer-term side-effects. To address this, we are carrying out a review to look at the evidence of topical steroid safety in eczema from longer-term studies. Unlike the Cochrane systematic review which only includes randomised controlled trials, this review will include observational (non-randomised) studies as well as randomised controlled trials that report long-term safety of topical steroids for eczema.
Overview of existing reviews of topical steroid safety
There are a huge number of studies looking at topical steroid use in people with eczema so it will take some time to do the Cochrane and long-term studies systematic reviews. So in the meantime, we are conducting an overview of existing systematic reviews of the safety of topical corticosteroids. This overview is dependent on the content and the quality of the reviews already published, but it will provide a useful summary of the evidence in the interim. The results of this overview will be available shortly.
How will we use the information from these reviews?
The findings from all three systematic reviews will be used in the ECO interventions we are developing. We will share the results widely and in different formats including video blogs and short summaries for people with eczema and their parents /carers, and for healthcare professionals. Our international team of patients, clinicians and methodologists carrying out these reviews will ensure the findings are applicable around the world.
Jo Chalmers
Qualitative research is key for finding out people’s views and experiences, using methods such as interviews to explore the ‘How’ and ‘Why’ of research questions. In ECO we will be carrying out lots of qualitative interviews with parents, children, and young people with eczema. ECO also builds on previous qualitative work that we have done and also on the work of Matt Ridd, Kingsley Powell, Emma Le Roux, and many others.
Although we are still doing more qualitative research, we have already interviewed many families of children with eczema to find out about their perspectives and would like to highlight some of the findings in this blog.
Parents of children with eczema had really varied experiences of seeking information about eczema online with some saying they couldn’t find much about it, and others feeling overwhelmed by the quantity, or unsure about commercial interests online, for instance clothing, creams or online allergy tests.
Looking at the information that people exchange in online discussion forums (sites like Mumsnet) also showed there is a lot of confusion, particularly around safe use of topical corticosteroids. People sought advice from other online forum users and, although some attempted to reassure others that topical corticosteroids can be used safely, the overall discussions seemed likely to exacerbate concerns and confusion.
This suggests that health professionals have a key role in signposting people towards high quality information to back up topics discussed in the consultation, or address concerns arising after the consultation.
Health professionals contribute to mistrust in topical corticosteroids
Many parents of children with eczema said they were really concerned about having received conflicting advice from different health professionals about what is ‘safe’ use of topical corticosteroids. It is unsurprising that parents therefore tend to feel cautious or confused about using them. These suggests that health professionals need to think harder about how they communicate key messages and providing links to reliable information could help here too.
We found that many parents of children with eczema feel a mismatch between their concerns and those of their GPs around topics such as interest in food allergy, feelings around a ‘trial and error’ approach and generally feeling ‘fobbed off’ by prescriptions for emollients and an assurance that their child would ‘grow out of it’. Again, this suggests a need for better communication, and provision of high quality information for families.
The range of strategies families develop to deal with this is impressive, including involving the child in treatment, distracting the child during treatment, making a game of it, using rewards, applying treatment to a sleeping child or, in a few cases, physically restraining the child or reducing frequency of applications. Clearly families met with varying success, but development of habitual confrontation appears to be common and support in dealing with this would be welcome.
The conclusions of these papers reiterates the key role of health professionals in signposting people towards high quality evidence-based support and information addressing the range of challenges that eczema presents on a daily basis. We hope that ECO is going to help to make this happen.
We have an action packed 5 years ahead in which we will carry out further qualitative interviews with children, young people, and parents. We are also systematically reviewing all the previous qualitative research about eczema and exploring the views of teenagers and young adults with eczema through looking at HealthTalk data on eczema.
Miriam Santer and Ingrid Muller
Powell K, Le Roux E, Banks J, Ridd MJ. GP and parent dissonance about the assessment and treatment of childhood eczema in primary care: a qualitative study. BMJ open. 2018 Feb 1;8(2):e019633.
Le Roux E, Powell K, Banks JP, Ridd MJ. GPs’ experiences of diagnosing and managing childhood eczema: a qualitative study in primary care. Br J Gen Pract. 2018 Feb 16:bjgp18X694529.
Santer M, Muller I, Yardley L, Burgess H, Ersser SJ, Lewis-Jones S, Little P. ‘You don't know which bits to believe’: qualitative study exploring carers’ experiences of seeking information on the internet about childhood eczema. BMJ open. 2015 Apr 1;5(4):e006339.
Teasdale EJ, Muller I, Santer M. Carers' views of topical corticosteroid use in childhood eczema: a qualitative study of online discussion forums. British Journal of Dermatology. 2017 Jun 1;176(6):1500-7.
Santer M, Burgess H, Yardley L, Ersser S, Lewis-Jones S, Muller I, Hugh C, Little P. Experiences of carers managing childhood eczema and their views on its treatment: a qualitative study. Br J Gen Pract. 2012 Apr 1;62(597):e261-7.
Santer M, Burgess H, Yardley L, Ersser SJ, Lewis‐Jones S, Muller I, Hugh C, Little P. Managing childhood eczema: qualitative study exploring carers' experiences of barriers and facilitators to treatment adherence. Journal of advanced nursing. 2013 Nov 1;69(11):2493-501.
http://healthtalk.org/young-peoples-experiences/eczema/topics
I have had eczema all my life. My mother did too. And my children. It is because of my children’s struggles with eczema that I got involved with the Nottingham Support Group for Carers of Eczema. It is run in partnership with the health care professionals in the local dermatology department. For the first ten years we held meetings at the local hospital. A carer attending for the first time usually did a lot of crying. Crying because it was a relief to find people who understood the daily struggle against eczema.
There is so much misinformation out there: friends, family, social media. What everyone needs is good quality, evidence based ideas which will make a difference. The NSGCCE is now a web-based support group and we have over 6400 followers on Twitter ( @eczemasupport). We have lots of information on our website. But the learning resources which ECO are looking to develop for the web will be really useful because the ECO team hope to structure and prioritise their information in a really user-friendly way. Giving those with eczema in their family something that helps them understand what is likely to have the biggest chance of giving them control of the eczema and their life back.
It is a great research team. It is amazing that all of them have come together, bringing their own expertise, to work on behalf of us. As a co-applicant, I am involved in lots of telephone conferenced meetings and even the occasional face-to-face. Basically being the constant reminder of eczema people. The team are always patient focussed, which makes my job really easy, but just occasionally they get hijacked by deadlines or research tasks (which are important if we are to produce a web-based learning resource that really works). So I am there to speak out for patients who are participants in this trial and those with eczema who will want to use the resource once it has been produced. Doing my small bit to make sure that ECO is a big deal for patients.
Amanda Roberts
Eczema Care Online is a programme of research funded by the NIHR (part of the NHS) aimed at improving the lives of people with eczema. It’s a big aim and we have big plans!
Why is this research important?
People who live with eczema have told us that they would have found it easier to get into an effective routine to control their eczema if they had received better information earlier on. Over 90% of eczema consultations take place with GPs, who often don’t have as much time or knowledge as they would like to explain everything (we know this because some of us are GPs). We have also met some people who are still a bit confused even after visiting specialist clinics in hospital.
If websites that support people to manage their eczema more effectively are proven to be helpful, then our hope is that health professionals will ‘prescribe’ their use as part of routine NHS care.
What will we do?
Over the next 5 years we will carry out the following research:
Project 1: Explore the support needs and barriers to self-care of people with eczema by reviewing existing evidence, and conducting interviews with people with eczema.
Project 2: Update and combine existing evidence around the safety and best ways to use topical corticosteroids and develop targeted advice for patients and healthcare professionals.
Projects 3 & 4: Develop eczema self-care support website/apps and test them to find out if they improve eczema.
Project 5: Plan how to promote eczema self-care support websites/apps in everyday use (if effective).
What has happened so far?
We are getting started with the extensive reviews in project 2 and enjoying getting out and meeting lots of people to help us with project 1, including visiting dermatology clinics, GP clinics, looking at all the existing research on concerns about eczema, interviewing children, young people and parents and carrying out an analysis of HealthTalk's fantastic resource of interviews with young people about their eczema.
Over the coming months we will post more blogs about how we are getting on. You can find out more, meet the team and follow our progress on our website or follow us (and the ECO whale) on twitter @ECO_eczema.
Miriam Santer and Kim Thomas (co-leads of Eczema Care Online)