Preclinical studies
Research areas
Introduction
Preclinical studies carried out by the Pain Centre Versus Arthritis have the broad remit of investigating the relationship between the arthritic joint and the peripheral and central processing of painful inputs originating from the joint.
A range of approaches are used in experimental models of arthritis pain, and molecular and analytical studies of clinical samples from people with arthritis are used to identify novel analgesic targets for the treatment of pain in arthritis.
Research areas
Joint structure, inflammation and pain
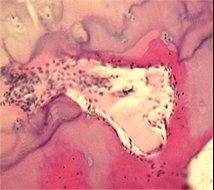
Pathological changes seen in human arthritis are associated with reported pain sensation. We are investigating the possible relationships between joint pathology and pain focusing on two models of OA. Modern quantitative methods of molecular biology and histology are used to explore how changes in the joint accompany changes in pain processing and pain behaviour. Interventional studies that inhibit innervation at the osteochondral junction, reduce synovitis and modify OA structural severity are being studied to determine their ability to modify pain behaviour. We are investigating how treatments that improve arthritis in the joint may reduce pain behaviour even after discontinuation of treatment.
Primary afferent neurones and arthritis pain
Aberrant peripheral nociceptive drive is thought to contribute to the pain of arthritis. The mechanisms underlying the changes in nociceptive drive include the sensitisation of those nerve fibres that innervate joint structures, leading to increased sensitivity to mechanical stimulation (reduced thresholds) and spontaneous firing. In man these functional changes may lead to activity-related pain, for example during walking or climbing stairs, and to pain at rest (ongoing pain) respectively. Why sensitisation develops in arthritis is not well understood. Furthermore, it is unclear which structures in the joint (such as its capsule and the subchondral bone) are the main sources of pain in arthritis.
Understanding the mechanisms of ‘peripheral sensitisation’ in arthritis is a fundamental aim of the pre-clinical work undertaken by the Pain Centre Versus Arthritis. Recent studies have demonstrated both electrophysiological and immunocytochemical changes in the primary afferent fibres innervating the joint in experimental models of OA pain. Similar experimental approaches are being undertaken to determine the effects of pharmacological interventions on the firing properties of afferent fibres innervating the joint.
Spinal mechanisms of pain in osteoarthritis
Clinical evidence suggests central sensitisation is a crucial feature of arthritis pain, which may also influence treatment responses both to pharmacological and surgical intervention. Current studies are determining the impact of joint pathology on the spinal and supraspinal processing of sensory inputs. Substrates with well-documented roles in the generation of central sensitisation are being evaluated in the experimental models of OA pain. We have expertise in a broad range of integrated in vivo approaches, including behavioural measures, electrophysiology (recordings of spinal neuronal activity and spinal nociceptive reflexes) and ex vivo molecular biology and analytical approaches. The aim of these studies is to advance our understanding of the pathophysiology of spinal and supra-spinal nociceptive processing in OA with a view to identifying new pharmacological targets for the treatment of arthritis pain.
Supra-spinal mechanisms of pain in osteoarthritis
There is mounting evidence that altered supra-spinal processing of sensory inputs contributes to altered pain responses reported in people with arthritis. Understanding the supra-spinal mechanisms of pain processing can be investigated using in vivo and ex vivo approaches. The University of Nottingham has a strong track-record in experimental and clinical functional imaging. Research undertaken by the Pain Centre Versus Arthritis builds upon this long-standing expertise in imaging. Functional magnetic resonance imaging approaches are being used to non-invasively investigate the supra-spinal processing of sensory inputs in experimental models of OA pain. Previously we have shown that these approaches can be used to detect changes in functional activity in discrete brain regions such as the insular cortex and primary somatosensory cortex in a model of neuropathic pain (Jones et al. 2009, Neuropharmacology, 56:2, 405-413).