Teaching methods
- Anatomy sessions
- Clinical skills sessions
- Case-based learning
- eLearning
- Full-body dissection
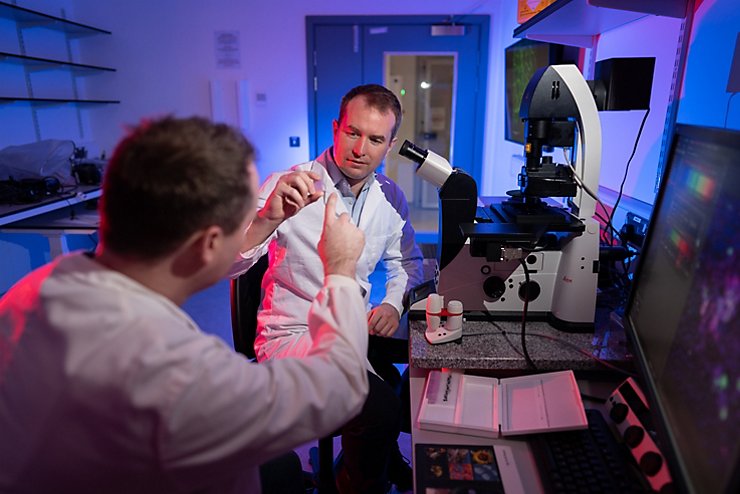
- Lab sessions
- Lectures
- Placements
- Practical classes
- Self-study
- Seminars
- Small group learning
- Tutorials

Medical School, Nottingham, UK
Please note that we are currently updating our undergraduate prospectus pages for 2025 entry, so the information below is subject to change. We expect to have our pages fully updated by the end of April 2024.
| Qualification | Entry Requirements | Start Date | UCAS code | Duration | Fees |
|---|---|---|---|---|---|
| BMBS | AAA | September 2025 | A100 | 5 years full-time | £9,250 per year |
| Qualification | Entry Requirements | Start Date | UCAS code | Duration | Fees |
|---|---|---|---|---|---|
| BMBS | AAA | September 2025 | A100 | 5 years full-time | £9,250 per year |
On graduating, you'll be able to provisionally register with the General Medical Council (GMC) for a licence to practice medicine in the UK. We'll help you through this process and provide support as you transition to the UK Foundation Programme.
To fully register with the GMC and be able to practice medicine unsupervised in the NHS or as part of a private practice, you will need to complete a Medical Licensing Assessment and complete the UK Foundation Programme.
Find out more about the GMC registration process
While most students continue in a traditional medical career to become doctors, a medicine degree can lead to careers in research, sales, journalism, illustration, communications, and economics and more.
On graduating, you'll be able to provisionally register with the General Medical Council (GMC) for a licence to practice medicine in the UK. We'll help you through this process and provide support as you transition to the UK Foundation Programme.
To fully register with the GMC and be able to practice medicine unsupervised in the NHS or as part of a private practice, you will need to complete a Medical Licensing Assessment and complete the UK Foundation Programme.
Find out more about the GMC registration process
While most students continue in a traditional medical career to become doctors, a medicine degree can lead to careers in research, sales, journalism, illustration, communications, and economics and more.
IB score: 36 (6, 6, 6 at Higher Level including Biology and Chemistry excluding core component).
7.5 (no less than 7.0 in any element)
As well as IELTS (listed above), we also accept other English language qualifications. This includes TOEFL iBT, Pearson PTE, GCSE, IB and O level English. Check our English language policies and equivalencies for further details.
AAA: must include biology (or human biology) and chemistry
A pass is required in science practical tests, where these are assessed separately. Please see below for full details.
A minimum of six GCSEs at Level 7 (A), including both Biology and Chemistry, you must have achieved a minimum of a grade 6 (B) in Maths and English Language. We do not accept GCSE resits. Please visit our undergraduate selection process page for full details.
Please note: Applicants whose backgrounds or personal circumstances have impacted their academic performance may receive a reduced offer. Please see our contextual admissions policy for more information.
Predicted A level grades, A levels, AS levels, or equivalent are not scored as part of the selection process. However, any offers made will be conditional on meeting the A level grades or equivalent required to meet the academic conditions of any offers. Please visit our undergraduate selection process page to read more about our selection process.
Your A levels must be studied over a maximum two-year period and three A levels have been passed at the required grades in one sitting.
A levels that have taken longer than two years to complete are not usually accepted.
This is to demonstrate your ability to manage a full academic workload.
We’ll also consider resits for no more than two A levels as long as you:
have completed your A levels in the last 12 months
have already obtained at least ABB with at least one A in biology/human biology or chemistry
must achieve AAA after taking your resits- this must include the other required science subject
IB score 36
IB requirements
IB score: 36 (6, 6, 6 at Higher Level including Biology and Chemistry excluding core component).
Please visit our undergraduate selection process page for full details.
GCSEs
A minimum of six GCSEs should be to have been studied over a two year period and that the required grades are achieved at one sitting
A minimum of six GCSEs at Level 7 (A), including both Biology and Chemistry, or double science and you must have achieved a minimum of a grade 6 (B) in Maths and English Language.
We will consider one GCSE subject resit in Maths, English Language, Biology, Human Biology, Chemistry or Double Science qualifications.
The achieved overall resit grade must be a minimum of Level 6 (B) in Maths or English Language, and a minimum of Level 7 (A) in Biology, Human Biology, Chemistry or Double Science (7,7) qualifications.
If you have not taken GCSE, iGCSE or equivalents because in the country where you have studied, GCSEs, iGCSEs or equivalents are not usually studied, please contact the University of Nottingham Enquires team for advice.
Please visit our undergraduate selection process page for full details.
UCAT
All applicants must sit the UCAT in the same year as the application is made for the course. Applicants who achieve a UCAT SJT grade of Band 4 will not be considered for this course.
Full details can be found on our undergraduate selection webpage.
We do not usually accept applicants who have studied Medicine before.
You cannot use other foundation courses at this university or any other medical school to transfer onto this course.
IELTS
7.5 (no less than 7.0 in any element)
English language requirements
As well as IELTS (listed above), we also accept other English language qualifications. This includes TOEFL iBT, Pearson PTE, GCSE, IB and O level English.
Non-UK entry requirements
Visa restrictions
International students must have valid UK immigration permissions for any courses or study period where teaching takes place in the UK. Student route visas can be issued for eligible students studying full-time courses. The University of Nottingham does not sponsor a student visa for students studying part-time courses. The Standard Visitor visa route is not appropriate in all cases. Please contact the university’s Visa and Immigration team if you need advice about your visa options.
Additional entry requirements
Non-UK entry
Please note: We accept degrees from international universities, and we require equivalencies to a UK degree as below:
If you’re currently studying for a degree:
You can apply for this course (A100) if you already have a degree. The entry requirements for this route are:
a 2:1 degree in any subject
the minimum A level requirements for this course
a minimum of GCSE level 4 (C) in maths and English language
If you’re currently studying for a degree, you can apply for medicine during any year of your existing studies. Do not withdraw from your current studies as your offer may be conditional on the completion of your current degree. If you chose this route, your A levels and GCSE’s must meet the course entry requirements.
If you need your degree result to be able to meet the academic entry requirements, you may apply through UCAS at the beginning of your final year of study. In these cases, your offer to study Medicine will be conditional on achieving the necessary academic requirements. Your current degree must:
be an honours degree
evidenced by sending ratified documentation (a copy of your final degree transcript or your certificate) by 20 July 2024
have been completed within the intended length of the qualification – for example, three years for a BSc or four years for an MSc
If you’re applying with an undergraduate (bachelors or undergraduate masters) degree.
You may not need to meet the standard A level requirements.
If you have achieved or are predicted to achieve a first-class honours degree at undergraduate level in a relevant subject with enough biology and chemistry content you may not have to meet the the A level requirements* . However, you’ll still need to achieve at least a 4 (C) in GCSE in both Maths and English Language.
Any offers made without the A level requirements are conditional on you achieving a first in your primary degree before starting the course.
If you have achieved or are predicted to achieve a first-class honours degree at undergraduate level in an non- relevant degree or undergraduate masters degree then the A-level requirement must still be met and they must have achieved a minimum of GCSE grade C (4) in English Language and Maths
Degrees must be completed in the natural length intended for the qualification (generally, 3 years for Bachelors, and 4 years for integrated Masters).
Accelerated degrees resulting in the award of a BSc Hons (completed over two years rather than three). These applications will be reviewed on a case-by-case basis. GCSE Maths and English Language must still be achieved at a minimum of a 4 (C) grade.
For more information on relevant degrees, please contact us.
Competition for places information can be found on our applying to Nottingham webpage.
Mature Students
At the University of Nottingham, we have a valuable community of mature students and we appreciate their contribution to the wider student population. You can find lots of useful information on the mature students webpage.
Alternative qualifications
Unfortunately, BTEC Nationals are not accepted for entry on to this course.
Unfortunately, the Access to HE Diploma is not accepted for entry on to this course.
Elite Athletes
We welcome applications from elite athletes for this course. Please visit our sports scholarships webpage for more information and full eligibility criteria.
To ensure your elite athlete status is recognized, please fill out the expression of interest in UoN Sport form before 15 October 2024, the UCAS deadline. This must be identified and confirmed to the Admissions Team by 21 December 2024.
Interview
You will be required to have an interview.
Interviews may be held face to face or online using Microsoft Teams: Further details will be available.
Mature Students
At the University of Nottingham, we have a valuable community of mature students and we appreciate their contribution to the wider student population. You can find lots of useful information on the mature students webpage.
Find out more about the Undergraduate Selection Process
Fitness to practice
We must be confident in your conduct, health and ability to be professional and interact safely with patients.
As part of your application, you'll be required to have an occupational health assessment and a disclosure and barring service (DBS) check.
We cannot accept pre-existing DBS checks. More information about this will be sent to you closer to your start date.
If we have any serious concerns we will not offer you a place, and reserve the right to revoke offers should serious concerns arise before starting the course.
Find out more about fitness to practise.
Excluded students database
When offering places to students we check the MSC Excluded Students Database as part of our commitment to professionalism and fitness to practice.
Applicants are usually expected to complete regular work experience when applying for medicine. This can be:
volunteering in a care related setting
volunteering with disadvantaged groups
paid employment in a job working with the general public
Please note, we are not expecting any in person NHS work experience. Your application for 2025 entry will not be negatively affected if you’ve been unable to complete any in person NHS work experience.
We will however be looking for knowledge of the profession and an understanding of the scope of the role of a doctor and we may ask about this during your interview.
If possible we'd advise that you speak to someone working in the NHS to ensure you are making an informed choice about your career in medicine.
We expect you to demonstrate a commitment to caring for people and a realistic idea of what working as a doctor entails.
Any students considering a gap year should use their time constructively either by working or further preparing yourself for a future career in medicine. The deadline for requesting a deferred start date for the Medicine A100 course is 1st May
AAA: must include biology (or human biology) and chemistry
A pass is required in science practical tests, where these are assessed separately. Please see below for full details.
A minimum of six GCSEs at Level 7 (A), including both Biology and Chemistry, you must have achieved a minimum of a grade 6 (B) in Maths and English Language. We do not accept GCSE resits. Please visit our undergraduate selection process page for full details.
IB score: 36 (6, 6, 6 at Higher Level including Biology and Chemistry excluding core component).
Please note: Applicants whose backgrounds or personal circumstances have impacted their academic performance may receive a reduced offer. Please see our contextual admissions policy for more information.
A level offer
Predicted A level grades, A levels, AS levels, or equivalent are not scored as part of the selection process. However, any offers made will be conditional on meeting the A level grades or equivalent required to meet the academic conditions of any offers. Please visit our undergraduate selection process page to read more about our selection process.
Your A levels must be studied over a maximum two-year period and three A levels have been passed at the required grades in one sitting.
A levels that have taken longer than two years to complete are not usually accepted.
This is to demonstrate your ability to manage a full academic workload.
We’ll also consider resits for no more than two A levels as long as you:
have completed your A levels in the last 12 months
have already obtained at least ABB with at least one A in biology/human biology or chemistry
must achieve AAA after taking your resits- this must include the other required science subject
IB score 36
IB requirements
IB score: 36 (6, 6, 6 at Higher Level including Biology and Chemistry excluding core component).
Please visit our undergraduate selection process page for full details.
GCSEs
A minimum of six GCSE’s should have been studied over a two year period and that the required grades are achieved at one sitting
A minimum of six GCSEs at Level 7 (A), including both Biology and Chemistry, or double science and you must have achieved a minimum of a grade 6 (B) in Maths and English Language.
We will consider one GCSE subject resit in Maths, English Language, Biology, Human Biology, Chemistry or Double Science qualifications.
The achieved overall resit grade must be a minimum of Level 6 (B) in Maths or English Language, and a minimum of Level 7 (A) in Biology, Human Biology, Chemistry or Double Science (7,7) qualifications.
Please visit our undergraduate selection process page for full details.
UCAT
All applicants must sit the UCAT in the same year as the application is made for the course. Applicants who achieve a UCAT SJT grade of Band 4 will not be considered for this course.
Full details can be found on our undergraduate selection webpage.
We do not usually accept applicants who have studied Medicine before.
Pease note that you cannot apply for both A100 or A10L and A108 in the same year of application.
Contextual offer information:
Please note: Applicants whose backgrounds or personal circumstances have impacted their academic performance may receive a reduced offer.
Applicants who meet the University of Nottingham Contextual Criteria may be eligible for a contextual offer of AAB with at least one A in Biology (or human biology) or Chemistry with the other no lower than a B.
Our IB contextual offer would be 35 points in total with 6,6,5 in Highers including 6 in either biology or chemistry, with the other no lower than HL 5. Scores exclude the core component.
Please see our contextual admissions policy for more information.
English Language
If your home country is not the UK but you are now living in the UK, with indefinite leave to remain and moved here after the start of school Year 10 from an international country where you were not studying the full curriculum (ie all subjects) in the English language:
And
If you have NOT achieved Level 6 (Grade B) GCSE English language, we will accept one of the following:
IELTS 7.5 (no less than 7.0 in any element)
Pearson Test of English (Academic) 79 (minimum 76)
Cambridge Proficiency/Advanced test (from January 2015) 191 with no element below 185
International Baccalaureate diploma: If GCSE hasn’t been taken and achieved at grade B(6) we require either IB English (standard level) at grade 6 or IB English (higher level) at grade 5.
Additional entry requirements
UK entry requirements
If you’re currently studying for a degree:
You can apply for this course (A100) if you already have a degree. The entry requirements for this route are:
a 2:1 degree in any subject
the minimum A level requirements for this course
a minimum of GCSE level 4 (C) in maths and English language
If you’re currently studying for a degree, you can apply for medicine during any year of your existing studies. Do not withdraw from your current studies as your offer may be conditional on the completion of your current degree. If you chose this route, your A levels and GCSE’s must meet the course entry requirements.
If you need your degree result to be able to meet the academic entry requirements, you may apply through UCAS at the beginning of your final year of study. In these cases, your offer to study Medicine will be conditional on achieving the necessary academic requirements. Your current degree must:
be an honours degree
evidenced by sending ratified documentation (a copy of your final degree transcript or your certificate) by 20 July 2024
have been completed within the intended length of the qualification – for example, three years for a BSc or four years for an MSc
If you are applying with an undergraduate (bachelors or undergraduate masters) degree.
You may not need to meet the standard A level requirements.
If you have achieved or are predicted to achieve a first-class honours degree at undergraduate level in a relevant subject with enough biology and chemistry content you may not have to meet the the A level requirements* . However, you’ll still need to achieve at least a 4 (C) in GCSE in both Maths and English Language.
Any offers made without the A level requirements are conditional on you achieving a first in your primary degree before starting the course.
If you have achieved or are predicted to achieve a first-class honours degree at undergraduate level in a non- relevant degree or undergraduate masters degree then the A-level requirement must still be met and they must have achieved a minimum of GCSE grade C (4) in English Language and Maths
Degrees must be completed in the natural length intended for the qualification (generally, 3 years for Bachelors, and 4 years for integrated Masters).
Accelerated degrees resulting in the award of a BSc Hons (completed over two years rather than three). These applications will be reviewed on a case-by-case basis. GCSE Maths and English Language must still be achieved at a minimum of a 4 (C) grade.
For more information on relevant degrees, please contact us.
Competition for places information can be found on our applying to Nottingham webpage.
Foundation progression options
If you don't meet the grades for this course and meet specific criteria for students from an underrepresented or disadvantaged background , you could apply for our Medicine at Nottingham with a Foundation Year (hyperlink https://www.nottingham.ac.uk/studywithus/ugstudy/courses/UG/Medicine-with-a-Foundation-Year-Bachelor-of-Medical-Scs-w-Hons-U6UMEDCF.html) (A108) course. It's the same great course, but it gives you an extra year to ensure you have the skills you need to succeed in Medicine. Please see our contextual admissions policy for more information.
You cannot use other foundation courses at this university or any other medical school to transfer onto this course.
Alternative qualifications
Unfortunately, BTEC Nationals are not accepted for entry on to this course.
Unfortunately, the Access to HE Diploma is not accepted for entry on to this course.
Interview
You will be required to have an interview.
Interviews may be held face to face or online using Microsoft Teams: Further details will be available.
Mature Students
At the University of Nottingham, we have a valuable community of mature students and we appreciate their contribution to the wider student population. You can find lots of useful information on the mature students webpage.
Elite Athletes
We welcome applications from elite athletes for this course. Please visit our sports scholarships webpage for more information and full eligibility criteria.
To ensure your elite athlete status is recognized, please fill out the expression of interest in UoN Sport form before 15 October 2024, the UCAS deadline. This must be identified and confirmed to the Admissions Team by 21 December 2024.
Find out more about the Undergraduate Selection Process
Fitness to practice
We must be confident in your conduct, health and ability to be professional and interact safely with patients.
As part of your application, you'll be required to have an occupational health assessment and a disclosure and barring service (DBS) check.
We cannot accept pre-existing DBS checks. More information about this will be sent to you closer to your start date.
If we have any serious concerns we will not offer you a place, and reserve the right to revoke offers should serious concerns arise before starting the course.
Find out more about fitness to practise.
Excluded students database
When offering places to students we check the MSC Excluded Students Database as part of our commitment to professionalism and fitness to practice.
Applicants are usually expected to complete regular work experience when applying for medicine. This can be:
volunteering in a care related setting
volunteering with disadvantaged groups
paid employment in a job working with the general public
Please note, we are not expecting any in person NHS work experience. Your application for 2025 entry will not be negatively affected if you’ve been unable to complete any in person NHS work experience.
We will however be looking for knowledge of the profession and an understanding of the scope of the role of a doctor and we may ask about this during your interview.
If possible we'd advise that you speak to someone working in the NHS to ensure you are making an informed choice about your career in medicine.
We expect you to demonstrate a commitment to caring for people and a realistic idea of what working as a doctor entails.
Any students considering a gap year should use their time constructively either by working or further preparing yourself for a future career in medicine. The deadline for requesting a deferred start date for the Medicine A100 course is 1st May
You're given a six-week 5 week elective placement at the end of your final year which you may choose to spend abroad. Elective placement destinations will depend on location restrictions (such as Covid-19, climate-related disasters, etc).
The course includes 15 main placements over the clinical phase, each lasting four to six weeks.
You're given a six-week 5 week elective placement at the end of your final year which you may choose to spend abroad. Elective placement destinations will depend on location restrictions (such as Covid-19, climate-related disasters, etc).
The course includes 15 main placements over the clinical phase, each lasting four to six weeks.
*For full details including fees for part-time students and reduced fees during your time studying abroad or on placement (where applicable), see our fees page.
If you are a student from the EU, EEA or Switzerland, you may be asked to complete a fee status questionnaire and your answers will be assessed using guidance issued by the UK Council for International Student Affairs (UKCISA) .
As a student on this course, you should factor some additional costs into your budget, alongside your tuition fees and living expenses such as travel and accommodation.
Approximately £53 for an enhanced DBS check (payable by the student). It is recommended to register the DBS with the government update service as soon as you receive it. The update service costs £13 per year.
You may need to buy some smart clothes to wear for clinical work settings.
You should be able to access the books and resources you need for the course through our libraries, however you may wish to purchase your own copies or get specific books which may cost up to £80 each.
In the final year of your course, students who live in the UK are eligible for NHS bursary funding (with some exceptions) which can help cover living costs and tuition fees.
Find out more about the NHS Bursary
As a student on this course, you should factor some additional costs into your budget, alongside your tuition fees and living expenses such as travel and accommodation.
Approximately £53 for an enhanced DBS check (payable by the student). It is recommended to register the DBS with the government update service as soon as you receive it. The update service costs £13 per year.
You may need to buy some smart clothes to wear for clinical work settings.
You should be able to access the books and resources you need for the course through our libraries, however you may wish to purchase your own copies or get specific books which may cost up to £80 each.
In the final year of your course, students who live in the UK are eligible for NHS bursary funding (with some exceptions) which can help cover living costs and tuition fees.
Find out more about the NHS Bursary
Home students*
Over one third of our UK students receive our means-tested core bursary, worth up to £1,000 a year. Full details can be found on our financial support pages.
* A 'home' student is one who meets certain UK residence criteria. These are the same criteria as apply to eligibility for home funding from Student Finance.
We are planning significant changes to our BMBS Medical degree programme from 2026 onwards, it’s important you understand these changes before applying to this course. Find out more
Doctors play a vital role in the lives of so many, from the most joyful, to the toughest moments. At Nottingham, we'll help you gain the clinical skills, knowledge and confidence to lead people through some of life’s most significant times.
Doctors play a vital role in the lives of so many, from the most joyful, to the toughest moments. At Nottingham, we'll help you gain the clinical skills, knowledge and confidence to lead people through some of life’s most significant times.
The early years
You’ll develop an understanding of the scientific and professional basics of medicine. You'll be taught subjects based on clinically relevant topics and patient examples. Areas of study will include, but are not limited to: respiratory, cardiovascular, cancer, musculoskeletal systems, gastrointestinal medicine, renal, endocrine, reproduction, and Central Nervous System.
From year one, topics studied in lectures, seminars, clinical skills, and anatomy suites are supplemented by patient interactions in hospitals or primary care settings. This part culminates in a research project and will see you graduate with a BMedSci degree after year three.
You'll be taught by experienced clinicians and tutors, research a topic from a broad selection of specialisms and benefit from being part of our Medical School, based at one of the UK’s busiest hospitals – the Queen's Medical Centre. Located just across the road from University Park Campus, meaning you’ll not only be part of our Medical School but also university life.
The later years
Also called the Clinical Phase, is where you’ll undertake a series of immersive placements at hospitals and GP surgeries. You’ll cover a range of specialties and experience medicine in different care settings, giving you a broad understanding and experience of how differently the NHS functions and cares for patients. At the end of the course, you will graduate with a BMBS, enabling you to work as a doctor on the UK Foundation Programme after you graduate.
Our in-depth but highly rewarding course provides you with an excellent start on your journey to becoming a doctor.
Important information
This online prospectus has been drafted in advance of the academic year to which it applies. Every effort has been made to ensure that the information is accurate at the time of publishing, but changes (for example to course content) are likely to occur given the interval between publishing and commencement of the course. It is therefore very important to check this website for any updates before you apply for the course where there has been an interval between you reading this website and applying.
Mandatory
Year 1
Biomedical Skills 1
Mandatory
Year 1
Integrated Medicine 1
Mandatory
Year 1
Medicine 1
Mandatory
Year 1
Medicine 2
Mandatory
Year 2
Biomedical Skills 2
Mandatory
Year 2
Clinical Medicine
Mandatory
Year 2
Integrated Medicine 2
Mandatory
Year 2
Medicine 3
Mandatory
Year 2
Medicine 4
Optional
Year 2
Complementary and Alternative Medicines
Optional
Year 2
Hearing Healthcare: From bench to bedside and back again
Optional
Year 2
History of Anatomy and Medicine
Optional
Year 2
Neuron Connectivity and Brain Function: From Development to Degeneration
Optional
Year 2
Risky Business: Understanding & Preventing Medical Error
Optional
Year 2
Laboratory Testing in Infection
Optional
Year 2
Translational Neuro-Oncology
Optional
Year 2
Physics of the Body
Optional
Year 2
Patient and Public Involvement in Research: "No research about me, without me"
Optional
Year 2
Pain: Aetiology, Consequences and Treatment
Optional
Year 2
Introduction to Sensory Neuroscience: Hearing Vision, Touch
Optional
Year 2
Drug Safety
Mandatory
Year 3
Clinical Pharmacology and Therapeutics
Mandatory
Year 3
Early Primary Care
Mandatory
Year 3
Evidence Based Medicine
Mandatory
Year 3
Honours Year Project
Optional
Year 3
Anti-Cancer Therapies and Cardiovascular Disease
Optional
Year 3
Cancer
Optional
Year 3
GPCR polymorphisms, disease and personalised medicine
Optional
Year 3
Improving your Chances of Publication
Optional
Year 3
Innate Immunity and the Immunopathology of Inflammation
Optional
Year 3
The Molecular Pathology of Cancer
Optional
Year 3
Patient safety, human error and avoiding harm in healthcare
Optional
Year 3
Respiratory Medicine
Optional
Year 3
Models and Approaches in Mental Illness
Optional
Year 3
Quantitative and Qualitative Methods for Mental Health Research
Optional
Year 3
Critical Thinking Skills in Epidemiology and Public Health
Optional
Year 3
Principles of Surgical Infection
Optional
Year 3
Developmental Neuroscience
Optional
Year 3
Clinical Applications of Current Neuroglia Research
Optional
Year 3
Malignant Haematology
Optional
Year 3
Clinical Renal Physiology and Therapeutics
Optional
Year 3
Introduction to Functional Medical Disorders
Mandatory
Year 4
Preparation for Practice
Mandatory
Year 4
Foundations for Practice
Mandatory
Year 4
Advanced Practice
The above is a sample of the typical modules we offer, but is not intended to be construed or relied on as a definitive list of what might be available in any given year. This content was last updated on Monday 15 April 2024.
This module provides students with the background to anatomy, radiology and imaging, coupled with a basic understanding of clinical measurements (biochemical, physiological, pharmacological and numerical) that will be essential for progress in clinical medicine.
This module enables development and assessment of the student’s capacity to integrate knowledge across all body systems to assess patient and symptom presentation permitting differential diagnosis.
The module will include understanding of anatomy, physiology, biochemistry and pharmacology as well as clinical testing and patient communication and treatment and will build upon knowledge and skills obtained from the case studies that overarch each week.
This module contributes to developing an understanding of the scientific and professional basis of medicine.
In particular, the module aims to develop knowledge and understanding of fundamental biochemical, physiological and anatomical concepts and their relation to disease processes.
The theme-based content will include:
You'll also be taught the basic knowledge, skills and attitudes required for the assessment and management of patients. As well as be introduced to the patient as a whole person. You'll be asked to consider challenging ethical scenarios and receive an introduction to ethical frameworks as well as considering issues such as information governance and confidentiality.
The module will provide you with some basic clinical skills and introduce them to theoretical and statistical approaches to understanding health. You'll also receive training in first aid for mental health. This is delivered by lectures, popular topics, directed reading, private study, workshops, e-learning, practical classes and hospital and general practice clinical visits to both primary and secondary care.
This module provides an introduction to the basic anatomy and physiology of the respiratory and cardiovascular systems, cancer biology and the musculoskeletal system, together with fundamentals in haematology.
The module teaches physiological control mechanisms, the pathophysiology and pharmacological approaches to treating common disease states. It also aims to develop knowledge and understanding of cancer biology and the anatomy of the neck shoulder and upper limbs.
In terms of professional development and communication, health beliefs and culture and communicating with people who are distressed are taught as well as how to interpret and communicate risks and screening and diagnostic testing. Students will be introduced to the concept of randomized controlled trials.
This module is delivered by lectures, seminars, practical classes, podcasts, directed reading, private study, workshops and clinical visits.
This module provides students with further background to anatomy, radiology and imaging, coupled with a basic understanding of clinical measurements (biochemical, physiological, pharmacological and numerical) that will be essential for progress in clinical medicine.
This module contributes to further development of an understanding of the doctor as a professional. Students will be taught the basic knowledge, skills and attitudes required for the assessment and management of patients. Students will be introduced to the patient as a whole person.
They will be asked to consider challenging ethical scenarios and will be taught how to communicate sensitively and empathetically with different patients in various scenarios.
The module will provide students with some basic clinical skills (e.g. taking a patient history, assessing gastrointestinal function) and introduce them to theoretical and statistical approaches to understanding health.
This is delivered by lectures, popular topics, directed reading, private study, workshops, practical classes and hospital and general practice clinical visits to both primary and secondary care.
This module enables development and assessment of the student’s capacity to integrate knowledge across all body systems to assess patient and symptom presentation permitting differential diagnosis.
The module will include understanding of anatomy, physiology, biochemistry and pharmacology as well as clinical testing and patient communication and treatment and will build upon knowledge and skills obtained from the case studies that overarch each week.
This module aims to develop knowledge and understanding of fundamental biochemical, physiological, pharmacological and anatomical concepts and their relation to gastrointestinal disease processes, endocrine physiology, the reproductive system and the kidney.
The module will provide an introduction to the alimentary system, and important aspects of nutrition and metabolism.
In addition, endocrine system teaching will provide the knowledge base for management of disease. This module will include the non-reproductive endocrine system with particular attention on pituitary, adrenal, thyroid and pancreatic function. As the endocrine system is a key system involved in whole body homeostasis, principles of control and integration of metabolism will be re-visited.
The reproductive system will cover the male and female reproductive system and pregnancy with particular attention on function of the ovary and testes, endometrial, cervical epithelial and prostate gland changes, placental physiology, problems in pregnancy and hormonal control of the reproductive system.
Renal teaching will provide descriptions of the intrarenal circulation and its relation to tubular elements, the processes located to the proximal tubule, loop of Henle, distal tubule and collecting duct, and the integration of these systems in the control of extracellular fluid volume and osmolality (including hormonal mechanisms) and in acid-base balance.
Students will be continue their general practice clinical visits. They will also be taught the skills of history taking and examination for patients with abdominal/alimentary conditions and they will be taught how to clearly explain information to patients. They will also focus on patients with an endocrine condition and will be taught diversity in sexuality and how to challenge attitudes of prejudice. Students will examine eyes and ears using an otoscope and ophthalmoscope.
Students will revisit the concept of safety, considering foresight, hazard awareness and risk. Students will also be introduced to measures of disease frequency and its relevance in clinical medicine. Physical and psychological changes and health behaviours that occur during adolescence will be explored. They will also be introduced to the concepts of systems and basic quality improvement approaches in healthcare. Further epidemiological analysis and the basis of evidence-based medicine will be introduced.
Topic specific communication skills will be explored. Having previously considered why errors occur they will explore the steps and role of incident analysis in healthcare, including Duty of Candour. They will also explore the role of nontechnical skills in healthcare with a focus on teamwork, communication, decision making and situation monitoring.
Delivery will predominantly be via lectures, podcasts, workshops, anatomical dissection classes, clinical visits, e-microscope histology and directed private study.
This module provides an introduction to the basic anatomy, physiology, pharmacology and psychology of the central nervous system.
The module aims to develop knowledge of these fundamental principles within the context of relevant weekly themes. The theme-based content will begin with a focus on depression and anxiety.
Students will be provided with a general introduction to the relevant brain anatomy followed by an in depth examination of the system physiology and pharmacology. The depression and anxiety theme will include individual sessions on the limbic system, emotion and mood, and treatment strategies. Ultimately, this will provide the basis for understanding theme based functions and the production of behaviours.
Subsequent weekly themes include:
Content will be delivered through lectures, podcasts, and practical classes on brain dissection, clinical neurological demonstrations and plenary lectures. Furthermore, the module also continues to consider the themes of patient safety and human factors as well as continuing with their primary care visits. Students will be expected to engage in directed reading and private study.
To introduce the students to the issues surrounding the use of complementary and alternative medicines, including legal issues, safety issues, and interactions with drugs.
This optional module considers key aspects of understanding how and why errors in day to day practice can arise and how different aspects of human cognition can influence decision-making in routine and critical moments of clinical care. The role of multiprofessional team working in influencing these factors in day to day practice will be explored, and the influence of the design of healthcare work systems, environments, technologies and other resources we access to support effective care will be discussed.
The content of the module is based on a curriculum mapping exercise against published national and international curricula. This draws together the basic science of Human Factors and promotes the concepts of systems thinking and design, which in turn will help underpin safe professional practice and critical future leadership as a qualified doctor.
The module is designed so that students can attain some of the outcomes specified by the GMC in Outcomes for Graduates (2018) in the areas of Professional values and behaviours Professional skills and Professional knowledge. These are detailed in the Module Learning Outcomes.
During the module 'Laboratory testing in infection' students will be building on previous learning and acquiring knowledge to extend and deepen their understanding of the variety and properties of infectious agents, the laboratory procedures used in isolation and identification of pathogens and antibiotic sensitivity testing, and how these can be applied to management of infection.
This will predominantly be within a laboratory environment employing practical exercises and tutorial sessions based around case studies and additional demonstration materials.
There is a requirement for additional self directed study to supplement the taught material and emphasize the importance of appropriate laboratory investigations for diagnosis and treatment of infection.
This module includes the following topics:-
Introduction to malignant brain tumours
Paediatric brain tumours
Neuro-oncological surgery
Introduction to the neuropathology of CNS tumours
Brain cancer evolution
Future Medicines for Brain Tumours
Neuro-imaging (interactive tutorial)
Digital brain tumour genomes (bioinformatics workshop)
Neuro-oncology clinic (observation) OR Neurosurgical theatre (observation)
Multi-disciplinary team (MDT) neuro-oncology meeting (observation)
The module includes the following topics:
Terminology, Modeling and Measurement
Energy, Heat, Work and Power of the Body
Muscles and Forces
Physics of the Skeleton
Pressure of the Body
Osmosis and the Kidneys (including artificial kidney)
Physics of Lungs and Breathing
Physics of Cardiovascular System
Electrical Signals from the Body
Sound and Speech
Physics of the Ear and Hearing
Physics of the Eyes and Vision
The module includes the following topics:
• Introducing Patient and Public Involvement (PPI).
• What difference does PPI make anyway' Personal perspectives.
• PPI across the research cycle: practical examples of research.
• Identifying what the blocks are in PPI with a focus on diversity and inclusion.
• Skill and behaviours: running a PPI session.
• Writing a lay summary and running an online PPI session. Group project
During the module 'Pain: aetiology, consequences and treatment' students will be building on previous learning and acquiring knowledge to extend and deepen their understanding of physiological, anatomical, pharmacological molecular and cellular aspects of pain and to gain knowledge and understanding of the mechanistic basis of this neurological condition. This will also enable students to appreciate the clinical relevance of pain to patients and how it is currently managed. This will predominantly be within the setting of a series of lectures, but there is also a requirement for substantial private study to consolidate understanding of the material covered in the lectures.
This module includes the following topics:-
Signal transduction processes
Coding of sensory information and neuronal representation,
Corneal and retinal anatomy and physiology,
Early visual cortex
Visual memory
Ear anatomy and function
Peripheral auditory processing
Central auditory processing
Skin and the somatosensory system
Multisensory integration
Sensory impairment and disease, including practical
Major classes of clinical management
Contemporary research
Course Review
This module will explore the safety issues associated with Clinical Pharmacology and Therapeutics, which underpins safe and effective prescribing. The module will cover key adverse drug reactions, drug interactions, prescribing errors, applied pharmacokinetics and some key examples of drug safety issues.
This module will help you develop your prescribing skills and understanding of therapeutics and treating infections to prepare you for the Clinical Phase.
This module covers the aspects of primary care for young patients.
The aim of this module is to introduce the concept of evidence based medicine and review in depth many of the research methodologies, which underpin this. This will include ethical issues in animal and human research studies.
During the evidence based medicine course students will be building on previous learning and acquiring knowledge, skills and attitudes that link to aspects of the Outcomes for Graduate specified by the GMC. They will learn about the design of biomedical studies of various kinds, and the collection, analysis and interpretation of data, how to search for scientific information and how to critique biomedical studies and research papers. They will develop an understanding of the ethical considerations in medical research and the principles of academic integrity.
Students will attend lectures and will be required to engage in private study, including the reading of scientific research papers.
It will be essential to demonstrate appropriate professional attitudes and behaviour.
In your chosen area for your research, you’ll spend year three working on your Honours Year project in which you will carry out your project to test the hypothesis formulated in the research methods module. The form of the project can vary and may be based on laboratory work, audit, patient studies or an extended literature review with proof of critical engagement. A submission of around 10,000 words is expected as your project write-up. A range of optional modules related to Research Project are shown below.
This module focuses on how cancer therapies have developed in recent years, and how the long-term cardiovascular effects of these treatments in cancer survivors should be considered.
Six lectures will cover: an introduction to cancer therapy, the role of VEGF in tumour angiogenesis, anti-VEGF cancer therapies, cardiovascular consequences of anti-cancer treatment, the role of alternative splicing and molecular targeting in cancer and future strategies for cancer therapy.
This module provides a clinical overview of cancer including:
This module aims to facilitate:
This will predominantly be within the home base and there is a requirement for students to carry out significant private study including reading advanced texts, review articles and research papers on specialist medical science topics.It will be essential to demonstrate appropriate professional attitudes and behaviour.
Gain a strong understanding of what makes a good clinical research publication.
You'll be taught how to critically appraise clinical research (including performing your own critical appraisal) and what to consider when writing an abstract (and assessed by writing your own abstract for a piece of clinical research). You'll also be directed on how to search for published research for practice and research purposes.
You will be build on previous learning and acquiring knowledge to extend and deepen your understanding of molecular and cellular aspects of innate immunity and gain knowledge and understanding of the mechanistic basis of inflammatory diseases.
This will also enable you to appreciate the development of novel forms of therapy for inflammatory diseases.
This module uses colorectal cancer as a paradigm of neoplastic disease and covers the molecular basis of cancer, the clinicopathological manifestation of disease and translational research.
This module considers:
The course focuses on the clinical knowledge and basic research approaches to investigate:
The module will explore theoretical, research and clinical approaches to the understanding of theaetiology and treatment of common mental illness/disorders such as mood and anxiety disorders, psychotic disorders, neurodevelopmental disorders and neurodegenerative diseases. It will draw upon international as well as local research in these fields at the University of Nottingham.
You'll gain knowledge and understanding of the following in common mental health:
The module 'Quantitative and Qualitative Methods for Mental Health Research' is designed so that students can acquire the concepts, skills and knowledge required to conduct and evaluate both qualitative and quantitative research in mental health and explore concepts and principles of psychiatry and applied psychology to enhance their evidence-based practice.
This module is intended to prepare students for interpreting the literature they will read as practising physicians.
This involves teaching them critical thinking skills and includes examination of three medical topics covered by the assigned papers.
These will include the following study designs:
Important issues in epidemiological research such as ethics and clinical constraints, case definition, research methods, power, bias and confounding and strength of evidence will be discussed, as relevant, for each paper.
Systematic reviews and national clinical guidelines will also be studied to understand the process of how these contribute to evidence based medicine. This will provide understanding of how individual research studies are brought together, evaluated for their quality. and combined to provide the recommendations and guidance that is used by healthcare professionals in practice.
The module includes the following topics:
This module will provide you with a conceptual framework relevant to embryonic, foetal, neonatal, childhood and adolescent growth and development. You’ll be introduced to the pervasive concept of human development as a programmed evolution in structure and function of the brain.
You’ll explore the need for development in human neuroscience with reference to brain embryology; pre-term birth, brain tumours; and epilepsies, and other current clinical research areas, from new-borns to teenagers.
The module will cover the following topics:
This module will provide an overview of normal haematopoiesis and current concepts in normal and cancer haematopoietic stem cell biology.
It will also:
Kidney disease is relatively common and its incidence is increasing because of the ageing population and increases in the incidence of obesity, diabetes mellitus and hypertension.
This module focuses on the pathology and treatment of kidney diseases. This will predominantly be within an overview of renal structure and function, the clinical features of, and diagnostic tools used in, kidney disease, the pathology,assessment and management of kidney diseases such as glomerular disease,vascular disease, nephrotic syndrome, and chronic kidney disease.
This module is designed as a multidisciplinary course to equip medical students with the essential knowledge regarding the definition, updated pathophysiology, diagnostic and treatment pathways for the most frequent Functional Gastrointestinal Disorders (FGIDs) and of the most frequently encountered neurological, rheumatological and respiratory functional disorders.
Topics to be covered include:
This module entails intensive work on self-awareness and communication skills. You will evaluate the development of their own self-awareness and communication skills within the framework of counselling professional development.
Emphasis will be placed on the need for continuous intrapersonal development and awareness of personal cultural conditioning for counsellor competence. This will be achieved in skills practice and group work tasks and discussions.
This phase provides students with the opportunity to acquire and develop professional knowledge, skills, values and behaviours through experiential learning in primary care settings, outpatient clinics, operating theatres, the emergency room and patients’ homes. This is combined with seminars and simulation-based learning.
This phase will comprise of an introductory week followed by five sets of six-week placements in medicine, surgery, specialty skills, mental health and community-based medicine.
Placements are integrated to allow students to maximise their learning in each setting. After two placements there will be a formative assessment week, and at the end of the five placements, students will have summative assessments. Students will progress to a 12-week block involving a two-week junior assistantship and 10 weeks of two or four-week Student Selected Modules (SSMs). Students will choose from a wide variety of SSMs from across Nottinghamshire, Derbyshire and Lincolnshire.
This final phase of the course is divided into two components: Advanced Practice 1 and Advanced Practice 2.
This part of the course is intended to prepare students for the transition to working as a Foundation doctor and enable appropriate preparation for the GMC Medical Licensing Assessment.
Advanced Practice will consist of an introductory week followed by a series of clinical placements including a formative assessment mid-way through between Advanced Practice 1 and 2. Topics covered will include: Health Care of Later Life; Leadership and Management training; Intermediate Medicine including Rheumatology; Cancer and Palliative Care; Child Health, Obstetrics and Gynaecology; Advanced Primary Care; Critical Illness; Advanced Medicine and Surgery. Upon completion of these clinical placements, a revision week will be held followed by the final summative examinations.
Teaching methods
Assessment methods
During your first three years, you'll have approximately 16 to 18 hours of teaching contact time with around 20 hours of independent study per week. You'll spend around five days on placement each semester.
During your time in the Clinical Phase, you'll spend between 35 to 40 hours across five days every week studying and on placements. You'll spend around three to four days on ward, clinic or GP placement visits per week plus 8 hours of independent study time. This will include some out of hours work.
Your holidays will also differ during the Clinical Phase from the standard student timetable. You'll have about six weeks' holiday in each of the clinical phases. This is usually taken as two weeks at Christmas, two weeks at Easter, and two weeks during the summer.
When you graduate with your BMBS degree, you should usually be able to provisionally register with the General Medical Council (GMC) for a license to practice medicine in the UK. We'll help you through this process and provide support as you transition to the UK Foundation Programme.
To fully register with the GMC and be able to practice medicine unsupervised in the NHS or as part of a private practice, you will need to complete a Medical Licensing Assessment and complete the UK Foundation Programme.
You can find out more on the UK Foundation Programme and the GMC to their websites.
Average starting salary and career progression
A doctor on the UK Foundation Programme can expect to start at £27,689 to £32,050.
As you gain experience as a doctor and develop your professional skills, you may progress on to senior clinical posts and earn up to £107,688 depending on your role and years of service.
96.50% of undergraduates from the school of Medicine secured graduate level employment or further study within 15 months of graduation. The average annual starting salary for these graduates was £35,089.
HESA Graduate Outcomes (2017- 2021 cohorts). The Graduate Outcomes % is calculated using The Guardian University Guide methodology. The average annual salary is based on graduates working full-time within the UK.
Studying for a degree at the University of Nottingham will provide you with the type of skills and experiences that will prove invaluable in any career, whichever direction you decide to take.
Throughout your time with us, our Careers and Employability Service can work with you to improve your employability skills even further; assisting with job or course applications, searching for appropriate work experience placements and hosting events to bring you closer to a wide range of prospective employers.
Have a look at our careers page for an overview of all the employability support and opportunities that we provide to current students.
The University of Nottingham is consistently named as one of the most targeted universities by Britain’s leading graduate employers (Ranked in the top ten in The Graduate Market in 2013-2020, High Fliers Research).
Our Medical School is based in Queen’s Medical Centre, one of the UK’s largest hospitals. There are dedicated clinical skills facilities including a dissection suite and teaching laboratories for medicine and healthcare students.


I love studying medicine at Nottingham because of the overwhelmingly friendly atmosphere. Everyone is so keen to support you on your journey to become a doctor. Outside of the fantastic academic course, there are so many extra-curricular opportunities to get involved in, a lot of which are co-ordinated by MedSoc. This is a student-run society that manages over 60 clubs and societies, organises a whole host of events and focuses heavily on welfare. I can’t recommend Nottingham Medical School enough.
Pascal Vogiaridis
current student, former MedSoc President (2020-2021)

Faculty of Medicine and Health Sciences
5 years full-time
Qualification
BMBS
Entry requirements
AAA
UCAS code
A10L

Faculty of Medicine and Health Sciences
6 years full-time
Qualification
BMBS
Entry requirements
BBC
UCAS code
A108

Faculty of Medicine and Health Sciences
4 years full-time
Qualification
BMBS
Entry requirements
N/A
UCAS code
A101

Faculty of Medicine and Health Sciences
3 years full-time
Qualification
BSc Hons
Entry requirements
AAB
UCAS code
B121
Faculty of Medicine and Health Sciences
3 years full-time
Qualification
BSc Hons
Entry requirements
ABB
UCAS code
B131

Faculty of Medicine and Health Sciences
4 years full-time
Qualification
MSci Hons
Entry requirements
AAA
UCAS code
B130

Faculty of Science
3 years full-time
Qualification
BSc Hons
Entry requirements
AAA-AAB
UCAS code
FC17

Faculty of Science
4 years full-time
Qualification
MSci Hons
Entry requirements
AAA-AAB
UCAS code
FC1R

Faculty of Science
4 years full-time
Qualification
MSci Hons
Entry requirements
AAA-AAB
UCAS code
CF71
Our webpages contain detailed information about all processes in your student journey. Check them out alongside our student enquiry centre to find the information you need. If you’re still struggling, head to our help page where you can find details of how to contact us in-person and online.
