Glioblastoma: new hope at Brain Tumour Research Centre of Excellence
Professor Ruman Rahman, Director of the Brain Tumour Research Centre of Excellence at the University of Nottingham, on how a world-first programme offers new hope on glioblastoma.
Brain tumours kill more children and adults under the age of 40 than any other cancer, and of these brain cancers, glioblastoma is the most common and the most aggressive. It’s incurable and very difficult to treat – even after surgery, cancer cells remain in the brain and glioblastoma always returns. There’s little we can then offer in terms of further treatment and patients typically expect to live only 12 to 18 months after diagnosis.
Brain Tumour Research is the UK’s leading charity dedicated to finding a cure to this terrible disease, and invests in long-term programmes that enable researchers to build knowledge and expertise and deliver treatments to transform the lives of patients and their families.
There are six Brain Tumour Research Centres of Excellence in the UK, and the University of Nottingham hosts the newest, which officially opened on 28 January 2026.
Discover more about our new research centre
Five-year research programme
We were awarded £2.6m to fund a five-year research programme that’s the first of its kind. We’re focusing on the infiltrative margin, the tiny area of cancer cells at the edge of the tumour. When glioblastoma is removed by brain surgeons, small clusters of cancer cells remain and the disease always comes back, close to the original tumour. We’ve discovered that the cells of the infiltrative margin are more similar to the glioblastoma that grows back than the biology of the original tumour. So, by studying the infiltrative margin in unprecedented detail, and identifying genomic and imaging features, we can make far earlier predictions of tumour recurrence, and identify drugs that will stop the cancer.
This work brings together the university’s expertise in medical imaging, genomics, AI and mathematical modelling, and builds upon our critical mass and interdisciplinary expertise in cancer research. The science behind us becoming a Brain Tumour Research Centre of Excellence is exciting and groundbreaking - and Nottingham is the best place to deliver it.
We’re already home to the long-established Children’s Brain Tumour Research Centre, and the Naaz Coker Ovarian Cancer Research Centre, which opened last year, while Professor of Oncology Nigel Mongan is part a $125m global project tackling cancer iniquities.
"The science behind us becoming a Brain Tumour Research Centre of Excellence is exciting and groundbreaking - and Nottingham is the best place to deliver it."
Professor Ruman Rahman
The birthplace of MRI
And we’re the birthplace of MRI, one of medicine’s greatest inventions, and continue to drive new advances in precision medical imaging – as my team were preparing the centre bid together, the university was awarded £28m UKRI funding for the UK’s most powerful MRI scanner.
It’s also significant that our Brain Tumour Research Centre of Excellence is based in the university’s purpose-built Biodiscovery Institute. As well as home to world-leading facilities and passionate people, the BDI is a true beacon of interdisciplinary research, with an open-plan, utilitarian ethos where labs, equipment and expertise are shared.
We’re also connected (literally, by a sky bridge) to the Queen’s Medical Centre (QMC), the Medical School and MRI suites, and NHS consultants in neurosurgery, neuro-oncology, neuro-pathology and neuro-radiology are an integral part of the Centre.
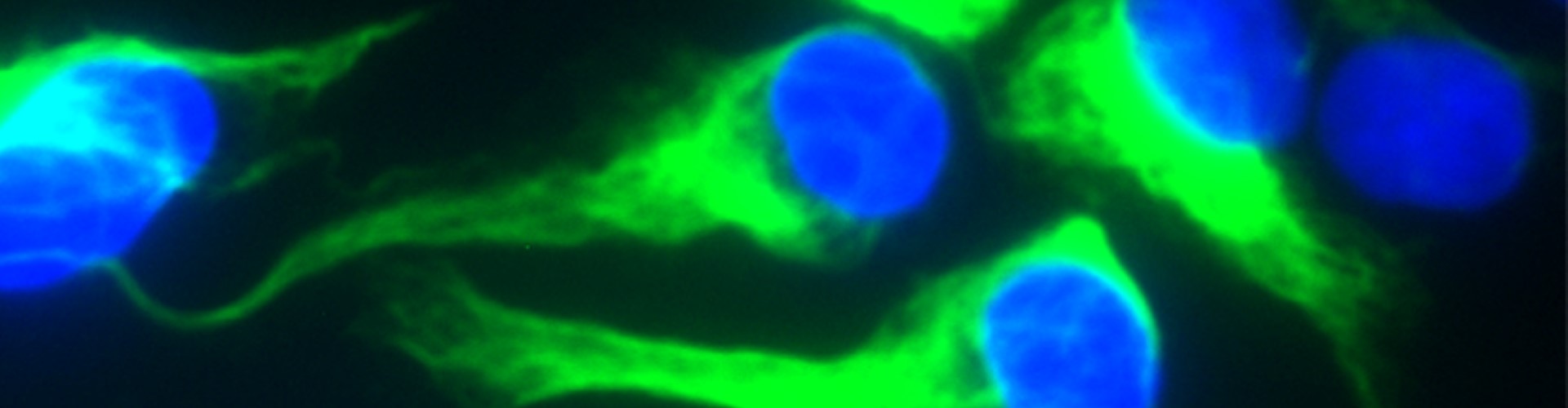
For our study, we are recruiting up to 50 glioblastoma patients at the QMC, who will be asked to undergo additional MRI brain scans upon consent, and we will integrate this enhanced data with genomic sequencing of biopsies of cells from the infiltrative margin, taken during surgery. (Interestingly, brain surgeons switch off the lights in the operating theatre and use pink fluorescent lighting to identify cancerous cells, which glow in the dark. (A trial of this now globally recognised technique was led by consultant neurosurgeon Dr Stuart Smith, and I remember going along to the QMC to watch.)
Exploring the infiltrative margin
The data from our advanced brain scans and sophisticated genomic sequencing will build an unprecedented picture of the infiltrative margin. Advanced MRI allows us to focus on the margin of the tumour, a tiny region containing the only cancer cells that survive current treatment. Standard scans, in the weeks following surgery, do not pick these up.
And with high resolution, single cell genomics we can sequence thousands of individual cancer cells, rather than just an average reading from the tumour mass, and see if a particular gene abnormally expressed is occurring in the majority of the 50 patients in our study.
Some of these genes might be crucially important as potential targets for therapy before the tumour even recurs. By adding the power of AI, and our expertise in mathematical modelling, we will be able predict tumour recurrence, with results based on an individual patient’s data.
During our five-year study, we expect to identify scores of potential drugs that could target the recurrence of glioblastoma after surgery, and following stringent testing in patient-derived cancer models, will narrow this down to one or two drugs, or a combination.
The unique long-term vision of Brain Tumour Research and sustained investment is key to our ambition of delivering a cure for glioblastoma. For every pound the charity invests in the university’s Brain Tumour Research Centre of Excellence, we pledge to find another £3 through additional funding and philanthropy.
Our inspiring patients and families
I’m humbled and inspired by the patients and families who are at the heart of the Brain Tumour Research Centre of Excellence at the University of Nottingham. At our opening, we unveiled a Wall of Hope, which will fill with tiles recognising supporters’ fundraising, honouring loved ones and charting our progress towards a cure. The altruism of the 50 patients taking part in our study is especially remarkable.
Our opening was also an opportunity for families and funders to take a tour of our labs and meet our team, including the PhD students and post-doctoral researchers who receive the majority of our funding and are the cancer research leaders of tomorrow.
And looking further ahead, our five-year research programme could inform another Nottingham-led revolution in MRI. As advanced imaging combines with AI to identify the biological features associated with glioblastoma, imaging for the disease could become routine in the NHS and may even circumvent the need for genomic sequencing. Imaging alone could also identify the drugs an individual would need for therapy. Now that would be transformative!
Bio
Ruman Rahman is Professor of Molecular Neuro-Oncology in the School of Medicine, based at the University of Nottingham’s Biodiscovery Institute.